Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 3012 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
UPDATED: There is no doubt that the book “De Humani Corporis Fabrica Libri Septem” written by Andreas Vesalius and published by Johannes Oporinus in May, 1543 is one of the most important scientific anatomical and medical books ever written. Much has been said about the place this book has in medical history as part of the discarding of dogmas and the establishment of scientific observation and thinking.
Some of the most intriguing images published in the book are fourteen woodcuts in the second book. These amazing and detailed images show the muscles in a whole body as it is dissected. The text details the structures and the procedure of how the dissection is performed.
It is believed that these images were done by Jan Stephan Van Calcar, an artist from the Titian’s studio, although there are indications that these images may have been authored by somebody else, or even that they were the effort of more than one artist working under the close supervision of Andreas Vesalius.
Today’s anatomical images are very descriptive and the artistry is relegated to the technique used for the depiction of the image. In Vesalius’ muscle men plates each image has a background showing a landscape. It was not until 1903 that it was discovered that the landscapes of the different images were part of a complete landscape. This is evident if these images are placed side by side. There have been several books and articles published on these images. Interestingly, some of the images had to be reversed to be placed in the panorama. This is due to the process of cutting the woodblocks.
The image in this article is one of two identified and composed by Harvey Cushing in 1943 (see sources). He calls it the "eight-series". The "six-series" can be seen here. To see Cushing's original template click here. The panorama of the six-series was identified by Cushing to be an area of the Euganean hills near Venice and Padua, Italy. There landscape formed by the eight-series is an actual region near Padua, Italy showing the ruins of old Roman baths. Cavanagh (1938) adds more information on these images, for his .pdf article, click here.
The image shown at the top of this article was created using original images from Vesalius’ Fabrica and composed using Adobe Fireworks CS5. Click on the image for a larger depiction. The large image is 1800px wide.
NOTE: In June 2023, I was able to purchase a single leaf of the 1543 Fabrica, page 187, which depicts one of the "muscle men". In the panorama image in this article it is figure number 3, from left to right. For more information on this image click here. This image is now properly framed in my office. Dr. Miranda.
This article continues here: "The landscape panorama of Vesalius' Muscle Men (2)"
Sources:
1. “A New View of the Vesalian Landscape” Cavanagh, GST Med Hist 1983, 27: 77-79
2. “The Panorama of Vesalius: A 'Lost' Design From Titian's Studio” Skandalakis, JE JAMA May 28, 1997, Vol 277, No. 20
3. “A Drawing for the Fabrica; and some Thoughts Upon the Vesalius Muscle-Men” Kemp. M. Med Hist. Jul 1970; 14(3): 277–288
4. “Andreas Vesalius: The Making, the Madman and the Myth” Joffe, SN. Persona Publishing 2009
5. "A Bio-Bibliography of Andreas Vesalius" Cushing, H. (1943) Schumann's
- Details
UPDATED: We have discussed many times on this blog the importance of Andreas Vesalius (1514 – 1564), his impact on modern science and anatomy, and the influence of his opus magnum publication in 1543, the Fabrica. The complete name of this publication is “De Humani Corporis Fabrica, Libri Septem” (Seven books on the structure of the human body).
Harvey Cushing wrote in his Vesalius bio-bibliography of 1943:”As a book, the Fabrica has been probably more admired and less read than any publication of equal significance in the history of science”.
The first (1543) and second (1555) editions of the Fabrica were published in Basel, Switzerland by Johannes Oporinus (1507 – 1568). With few exceptions, the Fabrica was sold as an unbound book and it was the owner’s responsibility to bind the book. One of the exceptions was the sumptuous purple silk-bound presentation copy delivered to the Emperor Charles V. As an interesting note, a Fabrica was discovered in Canada that was heavily annotated and as such had a low value. Who wants a book that of this importance that is so heavily hand-written? Analysis of the writing and style indicate that this copy belonged to Vesalius himself and was most probably the basis for a third edition that was never published. The annotations are used in the "New Fabrica" and if you are interested, here is a PDF file of a 2014 article on this topic.
Today we do not know how many books were actually printed as part of the first and the second edition of the Fabrica. Because of the time passed, lost or damaged books, during the last century efforts have been made to inventory the number of Fabricas still in existence, in studies made by Cushing in 1943 and Horowiz and Collins in 1984.The latest effort to account for the total number of these books was made by Stephen N. Joffe, MD, and Veronica Buchanan, MA in 2015 for both the 1543 and the 1555 editions of the Fabrica. Their papers were presented in February 2015 at the interdisciplinary symposium “Vesalius and the Invention of the Modern Body” in St. Louis, MO.
Dr. Joffe is the author of the book “Andreas Vesalius: The Making, the Madman, and the Myth”. Veronica Buchanan is the Archivist at the University of Cincinnati Henry R. Winkled Center for the History of the Health Professions.
The authors of these papers estimate that there are 64 complete copies surviving of the estimated 300 – 500 first edition printed in 1543. While a similar printing run is estimated for the 1555 edition, only 58 complete copies survive in the USA The papers can be read and downloaded on the following links:
"Updated Census in USA of First Edition of Andreas Vesalius’ ‘De Humani Corporis Fabrica’ of 1543”
READ DOWNLOAD
“An Updated Census of the Edition of 1555 of Andreas Vesalius’ De Humani Corporis Fabrica in the United States of America” READ DOWNLOAD
Note: The following link was sent to me by Dr. Elizabeth Murray and refers to the study by Joffe and Buchanan. The article “Accounting for an Historic Text” is from the University of Cincinnati Newsletter. Dr. Miranda
Sources
1. “Updated Census in USA of First Edition of Andreas Vesalius’ ‘De Humani Corporis Fabrica’ of 1543” Joffe, SN; Buchanan V. International Archives of Medicine; 2015: 8:1
2. “An Updated Census of the Edition of 1555 of Andreas Vesalius’ De Humani Corporis Fabrica in the United States of America” International Archives of Medicine; 2015: 8:1
3. Cushing, Harvey: A Bio-bibliography of Andreas Vesalius 2nd edition. Hamden: Conn.
4. Garrison, Daniel H., Hast, Malcom H.: Andreas Vesalius: The Fabric of the Human Body. Published S. Karger, Basel; 2014
5. "Andreas Vesalius; The Making, the Madman, and the Myth" Joffe, Stephen N. Persona Publishing 2009
- Details
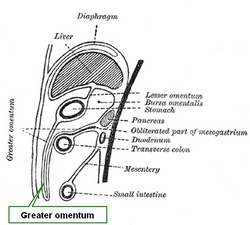
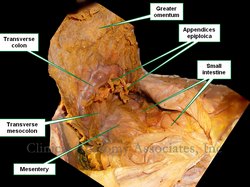
The [greater omentum] is a large, fatty apron-like structure that covers the abdominal viscera inferior to the greater curvature of the stomach. It is formed by a double peritoneal layer that contains fat, vessels, lymphatics, and nerves. This double peritoneal structure is continuous with the anterior and posterior serosal layers of the greater curvature of the stomach, drapes inferiorly, sometimes all the way to the pelvis and the folds upon itself posteriorly and superiorly ascending to become continuous with the anterior and posterior serosal layer of the transverse colon. Because it folds upon itself, the greater omentum can be considered to be a four-layered structure. See accompanying image.
The greater omentum contains vessels that arise from the right and left gastroepiploic arteries and veins as well as omental (epiploic) branches of the greater curvature vascular arcade.
The left border of the greater omentum reaches to the splenic hilum, while the right border extends as far as the pylorus and inferior aspect of the first portion of the duodenum. Because of its location, covering the intestines and its apron-like structure, the greater omentum is also known as the “surgeon’s apron”.
The term ‘abdominopelvic ligament” has been discussed in this article. The greater omentum has several “ligament” components that stretch between abdominal viscera. They are the:
• Gastrocolic ligament: Main portion of the greater omentum extending between the stomach and the transverse colon
• Gastrosplenic ligament: The portion of the greater omentum stretching between the stomach and spleen
• Splenorenal ligament: A continuation of the greater omentum stretching from the left kidney to the spleen.
As a side note, the lesser omentum (related to the lesser curvature of the stomach) contains less fat than the greater omentum.
First image(s) modified from the original by Henry VanDyke Carter. Public Domain
Second image(s) property of: CAA.Inc.. Photographer: D.M. Klein
- Details
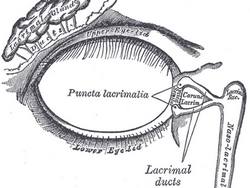
The root term [-dacry-] originates from the Greek word [δάκρυ] (d?kry), meaning “tear”, as in “a tear in your eye”. The equivalent Latin-derived root term is [-lacrim] from the Latin word [lacrima], meaning the same.
Here are some examples of the use of this root term:
- Dacryocystitis: Inflammation of the lacrimal sac. Look up [-cyst-], and [-itis]
- Dacryoadenitis: Inflammation of the lacrimal gland. Look up [-aden-], and [-itis]
- Dacryostenosis: Narrowing or blockage of a tear duct. Look up [stenosis]
- Dacryocystolithiasis: Presence of stones (calculi) in the lacrimal system. What is then a dacryocystolithectomy?
Image by Henry Vandyke Carter [Public domain], via Wikimedia Commons
- Details
The root term [-aden-] originates from the Greek word [αδένας] (adénas), meaning “gland”.
Glands are organs or groups of cells that internally secrete a substance and release it. When the substance is released into the bloodstream the substance will be known as a hormone and the gland as an endocrine gland. If the substance is released into an organ cavity or outside the body, the substance will have different names (sweat, sebum, mucus, etc.) and the gland will be known as an exocrine gland. Here are some examples of the use of this root term:
- Adenitis: Inflammation of a gland
- Adenocarcinoma: Cancer of a gland or a cancer that has a glandular look to it
- Lymphadenitis: Inflammation of a lymph gland (node)
- Lymphadenopathy: Disease of the lymph glands (nodes)
Note: The links to Google Translate include an icon that will allow you to hear the pronunciation of the word.
- Details
The complex suffix [-opathy] is formed by two combined suffixes. The first one is similar in origin to the root term [-path-] (basis for the medical term [pathology]); both arise from the Greek word [παθος] (pathos). Although Google Translate says it means “passion”, it also means “feeling”, “suffering” or a “distressed state” (Skinner, 1970). If we add the second suffix ending [-y] meaning “process”, a simple translation of the complex suffix [-opathy] is “disease process”, or “disease”.
It was first used by Galen of Pergamon (129AD – 200AD) as a term to denote a disturbance of a vital process. Vital processes were a convoluted attempt at explaining human physiology. Although wrong, Galen’s physiology was used for almost 1,400 years! You can read more on Galen’s physiological system here.
This suffix is widely used in medicine. Following are some examples:
- Cardiomyopathy: Disease of the heart muscle
- Myopathy: Muscle disease
- Nephropathy: Kidney disease
- Arthropathy: Joint disease
- Lymphadenopathy: Disease of the lymph glands (nodes)
Sources:
1. "The origin of Medical Terms" Skinner, AH, 1970
Note: The links to Google Translate include an icon that will allow you to hear the pronunciation of the word.