Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 3382 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
By Maurits Biesbrouck, MD. Continued from "Andreas Vesalius’s fatal voyage to Jerusalem (2)".
For the first page of this article, click here.
Title page of Jean Zuallart’s
Le tresdevot voyage de Iervsalem (1608)
This important letter was written in Monzon. Barón Fernández points out that it must date from the 24th of January, at the latest, as the monarch then left Monzon, after the sessions of the Cortes of Aragon were over. Vesalius was also in Monzon with the king. The king himself returned in January 1564, to Madrid, arriving there in May. So Vesalius must have received permission for his trip to Jerusalem while in Monzon, situated approximately 240 km from Perpignan, at the French border, while Madrid is 600 km from Perpignan. Presumably Vesalius left Spain directly via Monzon in order to avoid returning to the capital and making the far longer journey to France from Madrid. He definitely cannot have accompanied the king all the way back to the Spanish capital, as he was already in Venice by the 10th of March, as we shall see in the second letter.
But first some other important remarks. It is hard to imagine that the ultra-Catholic king would have written about Vesalius, to his ambassador, in such terms, if he had been condemned by the Inquisition, let alone, if he himself had had to intervene to protect him from the death penalty. If any of this had been true, we may suppose that the king would have expressed himself very differently. Second, the letter also undermines any claim that there was an ambivalent relationship between Vesalius and his king. Third, Philip II is apparently concerned about Vesalius’s welfare and takes safety measures. This was in no way excessive, as Jean Zuallart describes this journey as one of the most dangerous (10). Fourth, it is striking how Philip II expressly asks his ambassador to urge Vesalius to return swiftly. He will probably also have asked him this in person in Monzon, at the point when he gave him his permission to depart. It is just as if he was not entirely relaxed about the matter.
Letter 2: from Garcihernandez to Philip II
The second letter is the reply of Garcihernandez to the king, on March the 13th. Its translation reads: “Doctor Vesalius arrived here on the tenth of this month, and in order not to waste any time during his journey will, when conditions are favourable, sail from here to Cyprus, and will travel very well equipped, and in company, to Jerusalem. He says that he will travel as swiftly as possible. Ambassador Paulo Tiepolo and a brother of Giovanni Soranzo have very kindly helped him, to comply with [the wish of] Your Majesty. … Venice, the 13th of March 1564.” Signed: “Garcihernandez”.
So, in this letter Garciherandez states, that Vesalius had arrived in Venice on March the 10th, and would be sailing from there to Cyprus, with the support of several people. He stresses that no time will be wasted, and that he has conveyed to Vesalius the king’s wish that he should return as soon as possible. The theory that Vesalius used the journey, so that he could afterwards travel to Padua, seems to be undermined here, by the reply of Vesalius from Venice - albeit given indirectly -, that he will return to the royal court, as soon as possible.
Letter 3: also from Garcihernandez to Philip II
Fifteen days later, on March the 28th, ambassador Garcihernandez sent the king another letter, with only a short passage on Vesalius. Here we read in translation:
“Five hundred soldiers are being sent to Cyprus and a hundred to Corfu. The ships have remained in port because of the adverse weather, and Doctor Vesalius will be sailing in one of them, as I wrote to your Majesty...”
This short fragment means that Vesalius was still in Venice on March 28th, and that he was only waiting for better weather to embark.
Article continued here: Andreas Vesalius’s fatal voyage to Jerusalem (4).
Sources and author's comments:
10. Jean ZUALLART, Le tresdevot voyage de Iervsalem, auecq les figures des lieux saincts, & plusieurs autres, tirées au naturel, Anvers, Arnovld s’Conincx, 1608 ; see p. 85. First edition in Italian Il devotissimo viaggio di Gierusalemme (Roma, 1595).
- Details
By Maurits Biesbrouck, MD. Continued from "Andreas Vesalius’ fatal voyage to Jerusalem (1)".
Front cover of C. D.O'MALLEY,
Andreas Vesalius of Brussels 1514 1564,
Many other letters of Languet, in that period, to his friends and acquaintances were published but surprisingly in none of them he repeated the story, just as if it was of no importance (or even wrong) (4). We found it not even in his Historica descriptio susceptae a caesarea maiestate executionis... (Aug. 1567), in a copy of which North found his manuscript on the first flyleaf. In his biography of Hubert Languet the French biographer Henri Chevreuil found no mention of it either (5). The overall impression is that this short message is not more than a gossip written by Languet as a fait divers, perhaps who knows somewhat light-hearted after a couple of glasses on that first day of the new year. Apparently Languet didn’t believe in the story himself as he begins with the words ‘Fama est…’ (Rumour has it…) and he continues with the remark that the story with the direct motive for his Jerusalem travel is a remarkable (mirabilis) one. His letter concerns only that motive, thus things that happened some twelve months before, and were not at all very recent. He gives no details on Vesalius’s death itself. Languet and Peucer knew each other well. That same year 1565 Languet returned to Germany after a mediation of Peucer, but later on he returned to France (6). In any case it can not be regarded as a genuine letter, as such writings, for obvious reasons, normally treat on different subjects and are considerably longer. C.D. O'Malley, who gives an English translation too, calls this story "wholly unacceptable" (7).
The best and most detailed account of Vesalius’s last months is indeed to be found in O’Malley’s biography, but he was apparently not yet aware of the letters found by Barón Fernández. Yet it represents the first proper attempt to distinguish truth from fabrication. O’Malley was convinced that the ulterior motive behind Vesalius’ journey to Jerusalem was to escape the Spanish court and take up for a second time the chair in anatomy in Padua, which had fallen vacant, as a result of the death of Gabriele Falloppio, well before Vesalius’s departure.
The letters found by José Barón Fernández
After the congress of 1962 José Barón Fernández, a Spanish pediatrician, published his discovery of the four relevant letters, that he came across in the archives of Simancas (Spain), also in his Vesalius biography of 1970 (8). They were:
• a letter from the king of Spain to Garcihernandez, at his embassy in Venice;
• an answer from his ambassador ad interim;
• followed by an additional letter; and
• a letter from Bonifacio de Ragusa, custodian in Jerusalem, also addressed to the king (9).
Each of them concerns Vesalius’s trip to the Holy Land, a journey or pilgrimage, which was the subject of so much speculation.
Letter 1: from Philip II to Garcihernandez
This first letter is thus from Philip II, son of Emperor Charles V, and king of Spain, and is addressed to Garcihernandez, secretary to his ambassador, who was temporarily in charge of the Spanish embassy in the then powerful and wealthy Republic of Venice. The letter was written in Monzon, in Aragon, and dated January 1564. It reads in translation:
“ … Doctor Vesalius, who gives you this [letter], was the physician of the Emperor, my late father, and is now the same for me. He served his Majesty and likewise serves me, so that I have now very willingly allowed him and granted him permission, to travel to Jerusalem and visit the Holy Sepulchre of our Redeemer, in which he is motivated by piety. With my grateful consent, I expressly urge you, to help him on his way, so that he has a good passage, and to give him every help and assistance, …, so that he may swiftly travel there in safety, and remain there for as short a time as possible, in order that he may return with the same speed, so as to resume his service to me. Kindly encourage him to do this on my behalf. Monzon, January 1564.”
So, the king stresses that he gave Vesalius the permission to travel, and that the motive was his pious desire to visit the holy places. The Spanish ruler asks his ambassador to provide Vesalius with the necessary facilities for his journey, and to guarantee his safety, and also to ensure that he returns as soon as possible, in order to resume his service at the royal court.
Article continued here: Andreas Vesalius’ fatal voyage to Jerusalem (3).
Sources and author's comments:
4. Huberti Langueti Epistolae ad Joachimum Camerarium Patrem et Filium, Lipsiae et Francofurti, Mauritius Georgius Weidmannus, 1685. Also The Correspondence of Sir Philip Sidney and Hubert Languet, London: William Pichering, 1845. And Hubert Langueti ... Epistolae secretae ad principem ... Augustum Sax. Ducem ..., Halae Hermunduror., J. F. Zetler en H. G. Mussellus, 1699
5.Henri CHEVREUIL, Hubert Languet, Paris: L. Potier, 1856.
6. Oscar SCHOLTZ, Hubert Languet als kursächsischer Berichterstatter und Gesandter in Frankreich wärend der Jahre 1560-1572, Halle: Hermann Gesenius, 1875, 62 pp.
7. Charles Donald O'MALLEY, Andreas Vesalius of Brussels 1514 1564, Berkeley and Los Angeles: University of California Press, 1964, 8°, XV-480 pp.; see p. 304.
8. BARON FERNANDEZ, José. Andrés Vesalio: su vida y su obra, Madrid, Consejo Superior de Investigaciones Cientificas, Instituto “Arnaldo de Villanova”, 1970, 8°, XIX-312 pp., ill.; see pp. 234-248.
9. Ragusa is Italian for Dubrovnik in Croatia.
- Details
This article was written by Maurits Biesbrouck, MD. It is an expanded version of Dr. Biesbrouck’s communication on the International Conference Vesalius Continuum on the Ionian island of Zakynthos (Greece) on September 5th, 2014. This study is the result of a close collaboration with Dr. Biesbrouck’s colleagues and friends Prof. Omer Steeno and Dr. Theodoor Goddeeris, as a trio nicknamed ‘Cerberus’ by Theo Dirix, then the Consul of Belgium in Athens, and co-organizer of the conference with Pascale Pollier, Mark Gardiner and Ann Van de Velde.
In this overview I will try to tell something about the reasons for Andreas Vesalius’ travel, his stay in the Holy Land, his return voyage, the cause of his death, his burial place, and his epitaph. This text contains some new details and insights since our previous publications (1).
Title page of Barón Fernández’s
Vesalius biography (1970)
The legends
Many biographers wrote about the last months of Andreas Vesalius’ life. But because the necessary primary sources have been lacking, most of their stories should be regarded now as speculative. Thanks to the discovery of several letters in the archives of Simancas by José Barón Fernández in 1962 various points became clearer. As he presented the letters at the 19th International Congress on the History of Medicine in Basel in September of that year, it remains very strange that his important contributions remained unnoticed. Yet they were published at several instances in Spanish, a world language (2).
But first, something about the legends. The most persistent story, has it that Vesalius performed a dissection in Spain, on a nobleman whose heart was still beating when he exposed it, causing a great outcry. As a result Vesalius was condemned to death by the Inquisition, a sentence being commuted to perform a pilgrimage to Jerusalem, thanks to the intervention of Philip II, king of Spain.
There are numerous variants of this story, and anyone looking through the literature, invariably comes across one of these. Apart from this story - a legend as we must assume - here is a summary of the other so-called reasons that led Vesalius to travel to Jerusalem, according to different writers: for killing a woman; for dissecting a cleric’s mistress; because of an insatiable lust for wealth; to be away from his (quarrelsome) wife; troubles with the Galenist Spanish physicians; to escape from the tiresome Spanish Court; a promise after recovering from an illness; etc.
What is remarkable is that all these stories, without exception, only started to circulate after Vesalius’ death. It may be interesting however to look at the origin of the Inquisition story, the most tenacious one. This was caused by a short letter (merely twenty-four short rules) from Hubertus Languetus (1518-1581), a French diplomate, written in Paris on January 1st, 1565 to Caspar Peucer (1525-1602), physician and son-in-law of Philipp Melanchthon (1497-1560). That was ten weeks after Vesalius’s death. Michael J. North (Head of Rare Books and Early Manuscripts in the History of Medicine Division at the National Library of Medicine) had the lucky idea to reproduce a manuscript of it (3).
[Note: The manuscript is two pages and can be seen here: [Page 1]; [Page 2].
Here is a transcription:
De morte Vesalii ex literis Huberti Langueti, scriptis ad D. D. Casparum Peucerum anno Theos krononias 1565 Mense janu.
Fama est Vesalium esse mortuum audivisti proculdubio eum Hierosolymam esse profe ctum. Causa istius profectionis est mirabilis ut ad nos perscriptum est. Commissus erat eius curae viri nobilis in hispania, quem cum obiisse existimaret, nec satis causam mortis sibi percepisse videretur, petebat ab amicis uti sibi liceret corpus dissecare. Cumque pectus apperuisset, reperit cor palpitans. Cognati illius mortui non contenti erant illum accusare factae caedis accusarent impietatis apud inquisitionem existimantur se ibi vindictam vehementiorem assecuturos. Cum iam constaret de caede, nec tam facile excusaretur error medici tam periti, voluit omnino inquisitio de eo sumere supplicium. Vixque potuit autoritate sua vel potius precibus eum a tanto periculo eripere Rex ipse. Tandem concessum est Rei, et toti aulae pro eo deprecanti, ea conditione, ut ad expiandum illud scelus proficisceretur Jerosolymam ad montem Sinai. Vale. Datur Lutetiae calend Janu. anno a nato Christo 1565.
Translation
On the death of Vesalius, from a letter by Hubert Languet, written to doctor Caspar Peucer in January 1565 pcn.
Rumor has it that Vesalius is dead. You undoubtedly heard of his travel to Jerusalem. The reason for his departure, as it was written to us, is remarkable. In Spain the cure of a nobleman was trust to him. Thinking he was deceased, but not convinced about the cause of his death, he asked his friends to dissect the body. But on opening the chest he found the heart beating. The relatives of the deceased, not satisfied with an accusation for the committed murder, found it necessary to accuse him of godlessness before the Inquisition to obtain a more severe punishment. Once things became clear it was not so easy to excuse that error in a man of such an experience.
In short, the Inquisition intended to execute him. The King himself hardly succeeded to withdraw him from that great danger, relying on his authority or rather on his appealing. Eventually the King, and the entire Court that was pleading for him, were given in, on the condition that he should make a travel to the Mount Sion near Jerusalem, as a penalty for that crime. All the best, Paris, January 1st, 1565.
Article continued here: Andreas Vesalius’s fatal voyage to Jerusalem (2).
Sources and author's comments:
1. Maurits BIESBROUCK, Omer STEENO. ‘The last months of Andreas Vesalius. Part I - From Monzon (Aragon) to Jerusalem’ in Vesalius - Acta Internationalia Historiae Medicinae, 2010, 16 (no. 2): 100-106, ill.; IDEM, ‘The last months of Andreas Vesalius. Part II - From Jerusalem to Zakynthos (Zante)’ in Vesalius - Acta Internationalia Historiae Medicinae, 2011, 17 (no. 1): 30-34, ill. Also Maurits BIESBROUCK, Theodoor GODDEERIS, Omer STEENO. ‘The Last Months of Andreas Vesalius: a Coda’ in Vesalius - Acta Internationalia Historiae Medicinae, 2012, 18 (no. 2): 70-75, ill..
2.For the various publications on this subject by José Barón Fernández (and by others as well) see section ‘bibliography’ in www.andreasvesalius.be
3. Michael J. NORTH, ‘The Death of Andreas Vesalius’ in Circulating Now, U.S. National Library of Medicine, 15.10.2014, 2 pp., ill.; see http://circulatingnow.nlm.nih.gov/2014/10/15/ the-death-of-andreas-vesalius/. > Also https://www.facebook.com/nationallibraryofmedicine/ posts/10152749352150491.
- Details

Pavlos Plessas
Pavlos Plessas was born and brought up on the island of Zakynthos (Zante) in Greece. He lives in London but maintains an internet blog that explores the history of his native island. He is a historian of the island and an internet blogger.
Knowing the island, its history and its people he never believed that Vesalius was shipwrecked, left to die helpless and buried near the beach of Laganas. When the local interest in Vesalius was rekindled by the visit of Pascale Pollier and Theo Dirix, he tried to separate the evidence from rumours and speculation to see if a rational explanation of the mystery could be found.
He was approached by Pascale Pollier and Theo Dirix and asked to assist in their search for Vesalius' grave. With the help of local people and old maps he found the approximate location of the Santa Maria church, by which Vesalius had been buried. The scientific work of Dr. Sylviane Dederix confirmed that this was indeed the spot where the church once stood.
Thanks to Pavlos Plessas for collaborating with "Medical Terminology Daily" and allowing us to re-publish his work on "Powerful indications that Vesalius died from scurvy", presented originally at the 2014 "Vesalius Continuum" meeting in Zakynthos, Greece.
UPDATE: Pavlos' article and theory was refutted by Theo Dirix and Dr. Rudi Coninx. both contributors to this blog. Their article is entitled "Did Andreas Vesalius really die from Scurvy?". Not to be undone, Pavlos published his own rebuttal to their theory in the article "An answer regarding the death of Andreas Vesalius".
Following are some links to Pavlos Plessas' blog articles:
- Details
- Written by: Pavlos Plessas
Text from the presentation at the 2014 Vesalius Continuum Meeting in Zakyhnthos, Greece by Pavlos Plessas.
Continued from: Powerful indications that Vesalius died from scurvy (3)
Metellus mentioned another witness during Boucherus’ narration of their terrifying journey and Vesalius’ end. With him was his friend Johannes Echtius, an esteemed physician. Echtius was one of only a handful of doctors who had studied this new deadly disease, scurvy, and the very first person to write a treatise on it . In that treatise he had given the illness a name: scorbutus.
It is hard not to feel that this meeting between Echtius and Boucherus was not by chance, but, since nothing is known about it, any hypothesis made, however reasonable, will remain no more than a supposition.
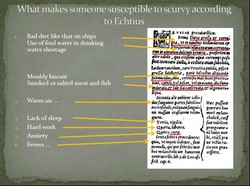
Fortunately, Echtius’ presence in that meeting gives us the opportunity to discern, through his friend’s letters, whether the 16th century expert believed that scurvy was Vesalius’ cause of death. Echtius had identified six conditions that made someone susceptible to scurvy, which he believed was contagious. The first was gross and corrupt diet, like the one on board ships, and the use of corrupt water in conditions of clean water shortage. The remaining five could all lead to scurvy independently, even if the diet had been good, because they generated an excess of melancholic humour, which in his opinion was the cause of the disease. As number five he had listed worrying.
It is easy to see what Metellus was pointing at when he accused Vesalius of having failed to provide adequately for himself. Pilgrims used to take with them their own supplies to complement the ship’s often unpalatable food. Echtius and Metellus believed that the ship’s food put Vesalius in danger of scurvy and he failed to take enough of his own. The subsequent shortages made things worse and, additionally, forced Vesalius to resort to drinking stale and foul water. His extreme worrying, after the disease appeared in others, made it almost inevitable that he too would contract scurvy. His sudden collapse and death did not come as a surprise either since this frequent scorbutic outcome is mentioned in Echtius’ treatise .
By expressing his conviction about the reasons that led to Vesalius’ death Metellus shows that he must have held a firm opinion on which precisely disease had killed him. Yet, incredibly, he fails in both his letters to name it expressly. Again, only scurvy can convincingly explain this failure. Echtius had written his treatise on scurvy in 1541 in the form of a letter , which for a long time had remained unknown even to some of the few doctors that had shown a keen interest in the disease. The treatise was not published until 1564, the year Vesalius died, in a book by Balduinus Ronsseus , and even then it was wrongly attributed to Johannes Wierus, who had sent it to Ronsseus. This error was only possible because Ronsseus, although he had been interested in scurvy for at least a decade , had not until then become aware of it. Consequently he had probably never come across the name scorbutus either. When the doctors of that time did not confuse scurvy with St Anthony’s fire, icterus niger, syphilis or leprosy, those who had a vague idea what they were dealing with, called it magni lienes, or stomacace and sceletyrbe. It would have been pointless for Metellus to inform his correspondents, a publisher and a theologian, that Vesalius had died from an illness Echtius called scorbutus when the word was meaningless even to well informed physicians.
Echtius may have been the world authority on scurvy but there were aspects of Boucherus’ story he must have found puzzling. The disease had broken out in the Mediterranean, an area that was believed to be free of scurvy. The diet of the crew had been bad, they worked hard and often spent the night sleepless – numbers 1, 3 and 4 respectively in his list of preliminary causes of scurvy – yet they did not get infected. Scorbutic Nostalgia remained unobserved for another two centuries, so Vesalius’ weird behaviour must have also caused him to wonder. Echtius then, along with Metellus, could not have invented this story, simply because they were unable to see that everything in it actually made sense. Neither could Boucherus have made up the story, because he knew much less about scurvy, if he knew anything at all. The probability that the events had been invented and put together randomly is absolutely negligible, given their perfect correlation with conditions that favoured an outbreak of scurvy, the timing of the outbreak, and the described symptoms; more so if all these are combined with the story having been afterwards presented to the planet’s most experienced scurvy expert.
Therefore, it is suggested that Metellus’ letters give a true account of Vesalius’ last days, and, simultaneously, that Vesalius, suffering from scurvy and seriously affected by scorbutic Nostalgia, managed to reach the southern part of the mythical kingdom of Odysseus – the land foremost associated with nostalgia since the dawn of history – and deposited there his own lifeless body.
Initial page of this article here.
Personal note: My sincere thanks to Pavlos Plessas for contributing this article to "Medical Terminology Daily". His theory and the evidence he presents is compelling, and although not proven, a powerful case is made for the cause of Vesalius' death at the gates of the port of Zakynthos, Greece. The fate and lost location of the illustrious anatomist's body is also researched in another article in this blog. I am proud to have been one of the many international attendees to the 2014 meeting in the island of Zakynthos. Dr. Miranda.
UPDATE: The case made by Pavlos Plessas is compelling, robust, and makes sense. Still, there are others that do not agree to his position, creating a discussion on the subject. In 2017, three years after his presentation in Zakynthos, Theo Dirix and Dr. Rudi Coninx published the article "Did Andreas Vesalius really die from scurvy?" which you can read here.
Sources and author's comments:
27. De Scorbuto, vel Scorbutica passione Epitome in 1541.
28. “… aliquoties vero desinit subito, ac mortali deliquio animi”.
29. The letter was addressed to a Dr Blienburchius of Utrecht. See Petrus Forestus, Observationum et Curationum Medicinalium, Tomus Secundus, Libri decem posteriores, Rouen 1553, p. 419.
30. De magnis Hippocratis Lienibus Libellus, Antwerp 1564, pp. 26a – 31b.
31. See De magnis lienibus Hippocratis, Plinique stomacace seu sceletryrbe epistola of 1555 in page 152 of Ronsseus’ De hominis primordiis hystericisque affectibus centones, published in 1559. I am indebted to Theodoor Goddeeris for pointing this out.
- Details
- Written by: Pavlos Plessas
Text from the presentation at the 2014 Vesalius Continuum Meeting in Zakyhnthos, Greece by Pavlos Plessas.
Continued from: Powerful indications that Vesalius died from scurvy (2)
Traditional herbal medicine from just north of Jerusalem reveals a not so unexpected legacy. Several plants are considered effective in the treatment of scurvy by local healers (14). This means that scurvy was well known in the area until recently. There is also more solid evidence from not too long ago: in a United Nations report from 1951 it is mentioned that not only many of the Palestinian refugees suffered from a mild form of scurvy but it was widespread amongst the general population of Jordan and Gaza (15). Gaza is by comparison much more fertile than Jerusalem. If the natives suffered from scurvy, what luck could the wandering foreigners have? When not on the road, living off preserved foods, pilgrims like Vesalius stayed and dined at monasteries. Fredrik Hasselquist, an 18th century naturalist, came across an outbreak of scurvy amongst the monks of exactly such a monastery, the one in Bethlehem (16). Hasselquist attributed their illness to eating salted fish and staying indoors.
In fact Vesalius, who travelled around in very high temperatures, was in a worse position than the monks. In a clinical experiment Michelsen and Keys showed (17) that, in conditions similar to those Vesalius would have faced, up to 4 mg of Vitamin C daily can be lost through perspiration, irrespective of dietary intake and concentration in the plasma. Vesalius would not have gone through the gruelling regime of the experiment’s subjects; however, the accumulative impact over his long stay in the area would have been significant.
It is by no means certain that Vesalius stayed in the Holy Land for three whole months. Hubert Languet wrote (18) that he intended to visit Mount Sinai, and Metellus hinted that he may have actually met Boucherus in Egypt. If this is true, he would have spent up to a month and a half in one of the harshest deserts on earth. His diet would have been similar to that on a ship: preserved or long lasting foods with perhaps some fresh meat, extremely poor in Vitamin C (19). His brief passage through the fertile Nile Delta would not have helped him much as he would have coincided with the annual inundation of the Nile, when almost all fertile land was either submerged or recently planted. The only fruit that would have been abundant in Egypt in early September is dates; but those contain virtually no Vitamin C (20).
Mentioning Vesalius’s symptoms was not in Metellus’ intentions. He did, however, mention two inadvertently. The first is Vesalius’ anxiety and fear, although Metellus considered them as one of the causes of his disease. Kinsman and Hood showed (21) that, in fact, personality changes and in particular hypochondriasis, depression, and hysteria, are the very first symptoms of scurvy. Such changes seem to have a physiological rather than a purely psychological basis according to Harrison (22). It is worth noting that, according to Solenander, Vesalius was taciturn by nature and melancholic, which may be an indication, that, unknown even to himself, he was already ill by the time Boucherus met him.
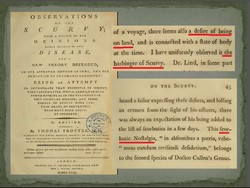
Depression was considered a cause rather than a symptom of scurvy for centuries after Vesalius’ death as we can see in a Sanitary Commission Report from the American Civil War. Alongside it another exciting factor is mentioned: nostalgia (23).
Thomas Trotter, who had called it (the depression) “Scorbutic Nostalgia”, observed it to be “the harbinger of Scurvy” and described it as “a desire of being on land” (24). Instinctively the sick person longed to be where the cure for his illness could be found. The most intriguing aspect of Vesalius’ altered behaviour was his fear of being buried at sea. It is as if his desire to be on land was so strong that he could not bear the thought of being away from it forever.
The second mentioned symptom is Vesalius’ collapse and instant death. The sudden death of scorbutic patients, often while they felt well enough to engage in some activity and while doing their utmost, has been observed and documented in several medical treatises and in accounts of long sea voyages (25). So many died after stepping out of the hold and onto the deck, or during and immediately after their disembarkation, that it was believed the change of air could kill a man with scurvy (26). This is exactly how Vesalius’ death is described: he dropped dead, soon after landing and while striving to complete the short walk to the first buildings of Zakynthos.
Article continued here: Powerful indications that Vesalius died from scurvy (4)
Initial page of this article here.
Sources and author's comments:
14. 6% of the plant species in use, according to Raeda Tawfeeq Ebrahim Daoud in Studies on Folkloric Medicinal Plants Used by Palestinians in the Qalqilia District, An-Najah National University, Nablus 2008, p. 32, table 3.3.
15. Assistance to Palestine Refugees, Report of the Director of the United Nations Relief and Works Agency for Palestine Refugees in the Near East, General Assembly, Official Records: Sixth Session, Supplement No 16 (A/1905), 28 September 1951, Chapter 1, 31.
16. Voyages and Travels in the Levant in the Years 1749, 50, 51, 52, London 1766, p. 147.
17. Olaf Mickelsen and Ancel Keys, The composition of sweat, with special reference to the vitamins, The Journal of Biological Chemistry, 1943, pp. 479 - 490.
18. Adam Melchior, Vitae Germanorum medicorum, Frankfurt Main 1620, p. 133. Also in a manuscript, with the title De morte Vesalii ex letteris Huberti Langueti, scriptis ad D. D. Casparu[m] Peuceru[m], National Library of Medicine, Bethesda, Washington DC (manuscript E 86).
19. According to Felix Faber, who travelled to the Holy Land in the last quarter of the 15th century, food on a pilgrim galley consisted of bread or biscuit, panada, cheese, eggs and mutton or fish; also lettuce with olive oil when they could find it. See Fratris Felicis Fabri Evagatorium in Terrae Sanctae, vol. 1, Stuttgart 1843, pp 136 – 137. In Vesalius’ time travelling in the Mediterranean in a sailing ship rather than a galley had become much more common. Those ships did not need frequent stops for water like the galleys, so fewer chances of lettuce salad. For his desert journey Faber used biscuit, smoked meat, smoked cheese, smoked fish, eggs, rice, almonds, oil, butter, vinegar, salt, wine, live poultry, raisins and onions. Information from the book Once to Sinai: The further pilgrimage of Friar Felix Fabri, by H.F.M. Prescott, New York 1958. Of these only onions contain appreciable quantities of Vitamin C when raw but hardly any if they are sautéed. For obvious reasons boiling was not very popular in the desert.
20. Deglet noor dates contain only 0.4 mg per 100 g. Medjool dates contain nil. Data from the United States Department of Agriculture
21. Robert A. Kinsman and James Hood, Some behavioral effects of ascorbic acid deficiency, The American Journal of Clinical Nutrition, April 1971.
22. Fiona E. Harrison, Behavioural and neurochemical effects of scurvy in gulo knockout mice, Journal for Maritime Research, Volume 15, Issue 1, 2013.
23. Report of a Committee of the Associate Medical Members of the Sanitary Commission on the Subject of Scurvy with Special Reference to Practice in the Army and Navy, Washington 1862, p. 17.
24. Observations on the Scurvy, 2nd Edition, London 1792, pp. 44 – 45.
25. For example Richard Walter, A voyage round the world in the years MDCCXL, I, II, III, IV, 5th edition, London 1749, p. 101 and James Lind, A Treatise on the Scurvy, London 1772, p. 132 and p. 281.
26. Thomas Trotter, Observations on the Scurvy, 2nd Edition, London 1792, p. 48.