Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 4764 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
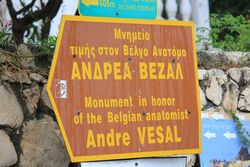
Continued from “The presence of Andreas Vesalius in Zakynthos (1)”
The second reminder of the presence of Andreas Vesalius in the Zakynthos Island is a street in the west side of the city of Laganas, “ΟΔΟΣ ΑΝΔΡΕΑ ΒΕΖΑΛ” or” Andrea Vesalius Street”. It is relatively short, narrow and windy, and it has several restaurants and hotels as you get closer to the sea where it ends at the beach. At this point there is a monument that honors Andrea Vesalius. This monument was erected in 1965. It has inscriptions in Greek, and Latin. This is the third memento to Vesalius in Zakynthos.

Vesalius Monument in Laganas
Vesalius Monument in Laganas
This monument was erected in Laganas following a legend that Vesalius had shipwrecked and he was found at the beach. Another legend says that Vesalius was left at the beach at Laganas to die as he was very sick. One of the presentations at the 2014 Vesalius Continuum meeting by Dr. Mauritz Biesbrouck disputed these legends with recently found letters by George Boucher to Johanes Metellus. George Boucher was a German jeweler that traveled with Vesalius back from Jerusalem and paid for Vesalius’ burial and monument at the church of Santa Maria della Grazie. These letters were authenticated and analyzed, bringing light to Vesalius’ place of disembarkment in Zakynthos. The Laganas monument, although correct in content, should be moved to the port of Zakynthos, to the point where the old city walls were found, the place where Vesalius collapsed and died.
The monument has a legend in both Greek and Latin. It reads as follows:
ΕΙΣ ΜΝΗΜΗΝ ΤΟΥ
ΑΝΔΡΕΑ ΒΕΖΑΛ
ΜΕΓΑΛΟΥ ΒΕΛΓΟΥ ΑΝΑΤΟΜΟΥ
ΘΑΝΟΝΤΟΣ ΕΝ ΖΑΚΥΝΘΩ ΤΟ 1564
Η ΕΝΩΣΙΣ ΤΩΝ ΔΙΠΛΜΑΤΟΥΧΩΝ ΤΩΝ
ΠΑΝΕΠΙΣΤΗΜΙΩΝ ΚΑΙ ΑΝΩΤΑΤΩΝ ΣΧΟΛΩΝ
ΤΟΥ ΒΕΛΓΙΟΥ, ΤΗΝ ΣΧΟΛΩΝ
ΑΝΗΓΕΙΡΕΝ ΤΘ 1965
IN MEMORIAM
ANDREAE VESALII BRUXELLENSIS
TUMULUS
QUI OBIIT IDIBUS OCTOBRIS ANNO MDLXIV
AETATIS VERO SUAE L
QUUM HIEROSOLYMIS REDISSET
Vesalii cineres venerandaque gentibus ossa
quisquis remota conteueris insula
qua jacer incultis memorosa Zakynthos arenis
gradum, viator et laborem sistito
naturae genium finemque extre maque rerum
vidisse credens coetera insanus labor
The rest is a poem in Latin that is translated as:
“The ashes and bones of Vesalius, sacred to the world
whoever finds then on this isolated island passing by the wild shores of Zakynthos,
should hold his tired steps, and believe that it is here that Vesalius met the ultimate goal of nature
and understood that striving for anything else is pointless” (Stouffis, Z, 1990)
When I visited this spot it was raining very hard and while I waited to take these pictures I looked out at the dark sea almost believing that maybe this was the spot where Vesalius came to land in Zakynthos. Now we know that it is not, but the moment was poignant and made me feel closer to the great anatomist.
On a more mundane note, in this area of Laganas because of the street name there are several businesses named "Vezal", a hotel, a supermarket and a taverna! I could not bring myself to post images of those places.
Continued in "The presence of Andreas Vesalius in Zakynthos (3)
- Details
The island of Zakynthos is one of the Ionian Islands found 155 miles (250 km) to the West of Athens. It is to the South of Macedonia, the island of Odysseus. It is also known as Zanthe or Zante, both pronunciations of the medieval Italian name for this island.
In October 15, 1564 Andreas Vesalius died suddenly at the gates of the main city of the island, also called Zakynthos, after a long and perilous return voyage from his pilgrimage to Jerusalem. The details of this trip and his potential cause of death will be covered in subsequent articles.
As famous as Vesalius is today, you would think that it would be easy to find information as to his grave and presence in the island. This is not so. Vesalius last trip to Jerusalem, his return, his death has been to date shrouded in mystery and legend. Some of these have been clarified in the 2014 Vesalius Continuum meeting in Zakynthos.

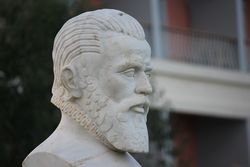
Plaque on the Bust of Vesalius in Zakynthos
There are a few reminders of the presence of Vesalius on the island. The first one is a marble bust found in a small triangular plaza found about 100 yards from the building of the Municipality of Zakynthos and the Dionysios Solomos Square(Πλατεία Διονυσίου Σολωμού). The plaza was initially called “Vesal square” and later was renamed after the former major of Zakynthos, Fotis Ladikos.
Described by O’Malley (1965) in his well-known Vesalius’ biography, I had a difficult time finding the bust, although it is on the main street in front of the sea looking at the port, as most locals do not know about it. It was only by chance that one of the attendees to the meeting, Dr. Kenneth Wise found it close to a well-known Greek Restaurant, the Gallo D’Oro (Golden Rooster). It was also by chance that he and I talked about it when discussing Dr. Wise’s book on Vesalius entitled “All Else Is Mortal”.
The marble bust has a barely readable marble plaque that reads in Greek:
ΑΝΔΡΕΑΣ ΒΕΖΑΛ
ΕΓΕΝΝΗΘΗ ΕΙΣ ΒΡΥξΕλλΕΣ 1-2-1515
ΑΠΕΘΑΝΕ ΕΝ ΖΑΚΥΝΘΩ 15-10-1564
ANDREAS VESALIUS
BORN IN BRUSSELS 1-2-1515
DIED IN ZAKYNTHOS 15-10-1564
This plaque has the wrong date of birth, as it is well documented that Andreas Vesalius was born on the early morning of December 31st, 1514, , making the year 2014 the 500th anniversary of his birth and the 450th anniversary of this death. This is the year when I spent a week in Zakynthos.
- Details

Fusiform gyrus.
Prosopagnosia ] is a neurological disorder characterized by the inability to recognize faces. It is also known as face blindness or facial agnosia. There are different degrees of presentation of this pathology and some patients go through life without knowing that they have this problem characterizing it as just “a quirk” or that “they just are not good at remembering faces”.
Advanced forms of prosopagnosia cause some patients not to be able to recognize their own face or their own family members. Prosopagnosia is thought to be the result of abnormalities, damage, or functional impairment in the right fusiform gyrus, located in the inferior occipitotemporal region of the brain. The fusiform gyrus is related to the limbic system and seems to coordinate the systems that control facial perception and memory. Prosopagnosia can result from stroke, traumatic brain injury, or certain neurodegenerative diseases
Prosopagnosia seems to also be congenital and run in certain families, pointing to a possible genetic disorder in the fusiform gyrus region.
The etymology of the term prosopagnosia is complex. It starts with the Greek word “gnosia”, a derivate of [γνώση] (gnósi) meaning “cognition”, “awareness”, or "knowledge". Adding the prefix “a-" leads to [agnosia] meaning lack or absence of cognition or awareness. The prefix "prosop-" derives from the Greek term [πρόσωπο] (prósopo) means f"ace". Therefore, prosopagnosia means “absence of facial awareness”.
There are famous people with prosopagnosia including Jane Goodall and Steve Wozniak.
Here is an interesting video from YouTube on the topic.
Image in the public domain, courtesy of Wikimedia. org.
Video courtesy of YouTube and Lucy Barnarf
Note: The links to Google Translate include an icon that will allow you to hear the pronunciation of the word
- Details
(UPDATED)
Say the following words out loud: "DISSECT" and "DISSECTION", then read on...
This is very high up on my list of personal annoyances or pet peeves. It was first brought up to my attention by Aaron Ruhalter, MD in his lectures. I was elated to find an article by Dr John H. Dirckx that took on the topic of the pronunciation of these terms. Dr. Dirckx states that the word should be pronounced with a short "i" as in "dissent"
The words “anatomy” and “dissection” are actually synonymous. Anatomy has a Greek origin. "Ana" means “apart” and “otomy” is the “process of cutting”: “to cut apart”.
Dissection has a Latin origin and means exactly the same! In fact, for many years the term “to anatomize” was used instead of “ to dissect”! Where is the problem? In the pronunciation! “Dissection” should rhyme with “dissent”, "kissed", and "missed"
An argument could be made that the wrong pronunciation (dai-ssect) is so prevalent that it should be accepted. I disagree, the wrong pronunciation of a word does not make it acceptable.
Further to this argument is a listing of words that include the term (-iss-) which you can read online here. I challenge the audience to find one instance, besides "dissect" and "dissection" where the term is pronounced "ais" instead of "iss".
Other pet peeves:
- Using the word "leg" to mean "lower extremity" as the leg is only a segment of the lower extremity: click here
- Using the term "ramus" instead of "ramus intermedius" for an anatomical variation of the cardiac vasculature: click here
- Using the term "thoratomy" instead of the proper term "thoracotomy": click here
... do not get me started on anatomical and terminological pet peeves... In fact, here is an article on "11+ medical words that are used incorrectly"
The image in this article is one of the few photographs that exists of Henry Gray. In this particular 1870 picture by Joseph Langhorn, Gray is in the anatomy laboratory (forefront, third from the left) at St. George’s Hospital with his students. At the time it was customary for medical students to pose in the anatomy lab with bones and cadavers. This is a practice not in use today which disappeared circa 1930. For anyone interested in this now considered gruesome custom, I would recommend the book "Dissection" by John H. Warner and James M. Edmonson.
Sources
1. "The Doctor's Dyslexicon: 101 Pitfalls in Medical Language" Dirckx, JH Am J Dermatopath 2005 Vol: 27(1):86. DOI: https://doi.org/10.1097/01.dad.0000148282.96494.0f
2. The Free Dictionary :https://www.thefreedictionary.com/words-containing-iss
- Details

Complete keratinization of the ocular surface
in a patient with ocular cicatricial pemphigoid
The term pemphigus refers to a rare group of autoimmune intraepidermal diseases characterized by blistering, pustules, or vesicles on the skin and mucous membranes. The mode of action of the disease is still not clear, but a key component is acantholysis, the disruption of the normal mechanisms of intercellular adhesion, which leads to intraepidermal blister formation.
There are several types of presentations of this disease such as p. vulgaris, p. foliaceus, p. vegetans, etc. One catastrophic presentation of this disease is ocular cicatricial pemphigoid. The pemphigoid disease progresses creating a symblepharon (adhesive attachments between the conjunctiva covering the sclera and the mucosa covering the posterior aspect of the eyelids. Eventually the disease may extend over the cornea. The accompanying image depicts a case of complete keratinization of the ocular surface in a patient with ocular cicatricial pemphigoid.
The root term pemphig- derives from the Greek [πεμφίγος] meaning a pustule or blister; the suffix -oid is also Greek [ειδής] meaning “similar to” of “kind of”. Therefore the medical term pemphigoid means “similar to blisters”
There is discussion as to when was this word first used, but it looks as though it was first published in 1763 in the book “Pathologia Methodica Practica, seu de Cognoscendis Morbis” by the French physician and botanist Francois Boissier de la Croix de Sauvages (1706 – 1767)
Sources:
1. “Revue D’Histoire Des Sciences” Louis Dulieu, 1969
2. "Etymology of Pemphigus" Holubar, K. J Am Acad Dermat 1989:21, 155-156
3. "Pemphigus" Korman, N. J Am Acad Dermat 1988: 18/6 1219-38
4. “Ocular Cicatricial Pemphigoid” Khan R,. McDermott M., Hwang, F. Am Acad Ophthalm Eye Wiki https://eyewiki.aao.org/Ocular_cicatricial_pemphigoid
Image courtesy of EyeWiki
- Details
The root term [-brachi-] comes from the Latin word [brachium] meaning "arm". Do not confuse with [-brachy-], which means "small" or "short".
It must be pointed out that there is an important discrepancy between the vernacular use of the term "arm" (as the whole upper extremity) and the anatomical "arm". In human anatomy the "arm" is only the portion of the upper extremity found between the shoulder joint superiorly and the elbow joint inferiorly. In some radiology studies, the arm is referred to as the "upper arm" so as not to include the forearm. This use of the term "upper arm" is incorrect and should be avoided by medical professionals.
Examples of the use of this root term in human anatomy and pathology are:
• Brachialis: A flexor muscle in the upper extremity
• Brachial plexus: A plexus of nerves related to the upper extremity
• Brachioradialis: A flexor muscle that extends from the arm to the forearm