Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1295 guests and no members online

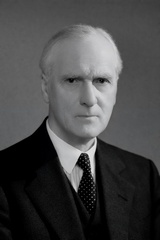
Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
- Written by: Efrain A. Miranda, Ph.D.
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Giovanni Paolo Mascagni (1755-1815). Italian physician and anatomist whose meticulous research and illustrations revolutionized the understanding of the lymphatic system. Born in the mid-18th century, Mascagni's career spanned teaching, research, and political turbulence, culminating in posthumous publications that solidified his legacy. However, his work was marred by a posthumous scandal involving theft and plagiarism by his former assistant, Francesco Antommarchi.
Paolo Mascagni was born on January 25, 1755, in Pomarance (near Volterra), Italy, to Aurelio Mascagni and Elisabetta Burroni. Some accounts place his birthplace in the nearby village of Castelleto. He received his early education at home, focusing on philosophy, literature, physics, and mathematics, before enrolling at the University of Siena to study medicine. Mascagni graduated with a medical degree in 1777. He was appointed assistant prosector to the anatomist Pietro Tabarrani (1702 - 1779). Following Tabarrani's death, he succeeded him as anatomy lecturer at the University of Siena.
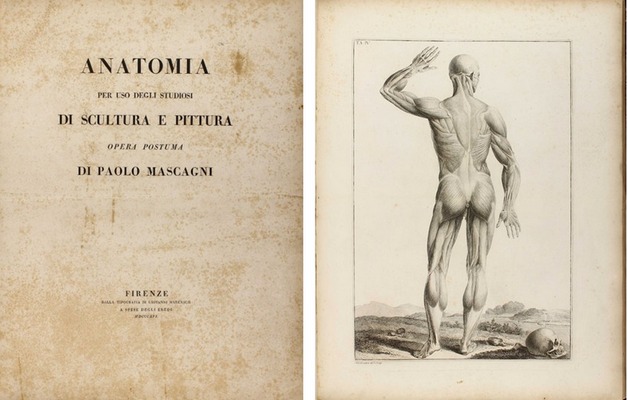
Mascagni's career was marked by academic accolades and political challenges. In 1796, he was elected a corresponding member of the Royal Swedish Academy of Sciences, and in 1798, he became president of the “Accademia dei Fisiocritici”(see end notes) in Siena. His Jacobin sympathies during the French occupation of Tuscany in 1799 led to his appointment as superintendent of arts, sciences, and charitable institutions, but after the French were expelled, he faced arrest and seven months in prison. Freed by royal decree in 1801, Mascagni was appointed professor of anatomy at the University of Pisa and a lecturer at the Hospital of Santa Maria Nuova in Florence. By 1807, he held the chair of anatomy at the University of Florence, where he also taught anatomy to artists, painters, and sculptors. As a result of his interest in human anatomy and art, the book “Anatomia per uso degli studiosi di scultura e pittura. Opera postuma” (Anatomy for the use of students of sculpture and painting) was published in 1816, one year after his death.
An accomplished artist himself, Mascagni collaborated with sculptor Clemente Susini (1754 – 1814) to create approximately 800 anatomical wax models, some of which are preserved in European museums: Museo La Specola, Florence, Italy; Museum Josephinum, Viena, Austria, etc. He also mentored Sardinian anatomist Francesco Antonio Boi (1767 – 1850), contributing to wax models now held in the Museo Archeologico Nazionale in Cagliari, Italy.
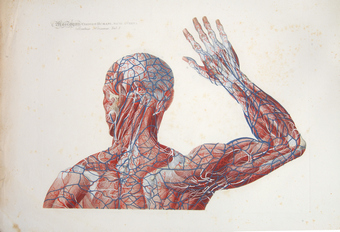
Mascagni's innovative techniques, such as injecting mercury into lymphatic vessels for visualization, allowed him to map a large part of the human lymphatic system, disproving earlier theories and highlighting its role in absorption and pathology. He is also credited with the early discovery of meningeal lymphatic vessels, later confirmed in modern studies (2014–2017). Mascagni died of sepsis on October 19, 1815, in Chiusdino, Italy.
Mascagni's publications blend scientific precision with artistic illustration. His 1784 work,” Prodrome d'un ouvrage sur le systeme des vaisseaux lymphatiques” (Initial notes on a work on the system of the lymphatic vessels), detailed his research on the lymphatic vessels and earned a prize from the Paris Academy of Sciences. This was followed by his 1787 publication “Vasorum lymphaticorum corporis humani historia et iconographia” (History and images of the lymphatic vessels of the human body), featuring 41 copperplates that provided the first complete description of the lymphatic system.
His most famous work was published after his death. He wanted to be able to depict the human anatomy in layers on a 5.9 ft. full-size person. Since this was not possible (see end notes), he worked with the artist and engraver Antonio Serantoni (1780 – 1837) to prepare three images of each plate in what is today known as the largest anatomy book ever published. Each page was printed in what is known as “double elephant folio”. To draw each plate, he dissected human bodies with the help of his assistant François (Francesco) Carlo Antommarchi (1780 – 1838).
After his death, with the help of family members and three professors on the Faculty at Pisa University (see end notes), his magnum opus “Icones Anatomiae Universae” (Images of Universal Anatomy”, was released in nine fascicles from 1823 to 1832, comprising 44 hand-colored copperplates and duplicates of each image (44 additional white and black pages) with symbols to identify each anatomical structure. The images depicted life-size layered views of the human body, from muscles to skeleton. These plates, engraved by Serantoni and others, covered the skeleton, viscera, cardiovascular and nervous systems, and more.
Because of the size, and the need to hand-color each of the 44 plates, and the publishing in fascicles, not many of these books were printed. The total number of the prints is unknown. What we do know is that today there are only 16 surviving complete copies of this incredible book, one of which can be seen at the Henry R. Winkler Center for the History of the Health Professions at the University of Cincinnati Medical College.
Following Mascagni's death, a scandal erupted involving his former prosector, Francesco Antommarchi. He took three sets of Mascagni's anatomical plates with him to St. Helena in 1815, where he served as Napoleon's physician. Upon Napoleon's death he stole Napoleon's death mask and passed it as his, attempting to make copies for sale. Defying a court ruling, Antommarchi published an unauthorized edition of Mascagni's book in Paris between 1823 and 1826. This version used 45 lithographed plates, omitting 24 figures from Mascagni's original and featuring inferior quality compared to the copper engravings. The theft and plagiarism by Antommarchi marred Mascagni’s vision. Only 8 of these books we published, one is lost, 6 are in private hands and the last one is in a library in Colombia.
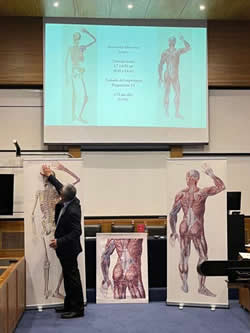
Dr. Miranda during his presentation at the
XLIII Anatomy Meeting in Chile
Personal note: Research on Paolo Mascagni has been important for me in the search for larger anatomical images. With the help of the University of Cincinnati Daniel Harrison Medical Library, I was able to use scans of Mascagni’s book and digitally join the images to present them as Mascagni intended. These full-size images are now part of my library and the library of my good friend Dr. Randall K. Wolf. The full-size image can also be seen at the Anatomy Learning Lab of the University of Cincinnati.
In 2023 I was invited to lecture on this topic at the Vesalius Triennial AEIMS, Antwerp – Belgium, and the same year at the XLIII Congreso Chileno de Anatomía.
End notes:
1. The “Accademia dei Fisiocritici” was founded in 1691 and is the second oldest scientific society in the world, second only to the “Fellowship of the Royal Society” of London, England, founded in 1660.
2. Andrea Vaccá-Berlinghieri (1772-1826) Professor of Surgery, Giacomo Barzellotti (1768-1839) Professor of Surgery, Giovanni Rosini (1776-1855) Professor of Eloquence. The publisher was Nicolaum Capurro.
Sources
1. “Mascagni. Paolo” Stefano Arieti. Dizionario Biografico degli Italiani - Volume 71 (2008)
2. "Art in science: Giovanni Paolo Mascagni and the art of anatomy". Di Matteo, N; Tarabella, V.; et al. Clin Orthop Relat Res. 2015 Mar;473(3):783-8.
3. "Books at Iowa: The Great Anatomy of Paolo Mascagni". Eimas, Richard
4. “The Anatomia Universa (1823) of Paolo Mascagni (1755–1815): The memory of a masterpiece in the history of anatomy after two centuries” Orsini, D; Saverino. D; Martini, M. Translational Research in Anatomy Vol 35, 2024, 100285 https://doi.org/10.1016/j.tria.2024.100285.
5. “The “prince of anatomists” Paolo Mascagni and the modernity of his approach to teaching through the anatomical tables of his Anatomia universa. A pioneer and innovator in medical education at the end of the 18th century and the creator of unique anatomica” Martini, M; Orsini, D. Italian Journal of Anatomy and Embryology.
6. “Una autobiografia inedita di Paolo Mascagni relativa specialmente al periodo delle rivoluzioni politiche avvenute in Toscana alla fine del sec. XVIII ed alle persecuzioni subite in tale epoca dal Mascagni stesso” Guerritore, T.G. 1928 Atti della Accademia dei Fisiocritici 10(3) 3-24
- Details
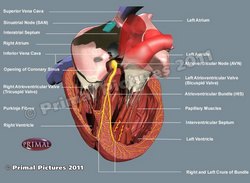
UPDATED: The sinoatrial node, is also known as the "sinuatrial node", "SA node" or by its eponym, the "node of Keith and Flack". It is the initial component of the conduction system of the heart.
It is a small nodule of cardiac muscle tissue, somewhat horseshoe-shaped that is found at the junction of the superior vena cava and the right atrium. Because of the inherent automaticity and rhythmical contractions of the SA node, it acts as the main pacemaker of the heart, being the base for normal heart beat, also known as "sinus rhythm"
It receives blood supply from the SA node artery, usually the first or second branch that arises off the right coronary artery. The SA node artery is a long vessel that passes between the right atrium and the ascending aorta on its way to the SA node.
The SA node receives innervation from both sympathetic and parasympathetic nerves. The parasympathetic innervation is by way of the vagus nerve, the Xth cranial nerve. The sympathetic innervation is by way of the cardiac nerves, a plexus that has its origin in the ventral rami of the first four thoracic spinal nerves (T1-T4).
The SA node was discovered in 1906 by Martin W. Flack (1882-1931) and Sir Arthur Keith (1866-1955). They named it originally the sino-auricular node.
Further studies by Cox (2020) have demonstrated that the SA node is not a single area of the right atrium, but rather expansive areas that beat at different beats per minute depending on the cardiac demand.
“Cardiac anatomy pertinent to the catheter and surgical treatment of atrial fibrillation”. Cox. JL et al J Cardiovasc Electrophysiol 2020 Aug;31(8):2118-2127. doi: 10.1111/jce.14440.
Click on the image for a larger version. Image modified from the original: "3D Human Anatomy: Regional Edition DVD-ROM." Courtesy of Primal Pictures
- Details
- Written by: Efrain A. Miranda, Ph.D.
The term “Bachmann’s bundle” refers to an eponymic structure associated with Jean George Bachmann (1877-1959) a French physician and physiologist. The proper anatomical term for this structure is “interatrial bundle” (Lat. fasciculus interatrialis).
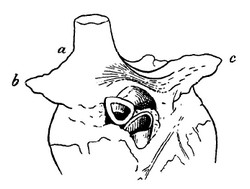
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. He measured activation times between the right and left atria and demonstrated that interruption of this distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction. The image, from his original publication, shows a dog’s heart with Bachmann’s bundle.
Bachmann’s bundle is a broad, flat band of atrial myocardium that crosses the superior aspect of the interatrial sulcus. It extends from the right atrium close to the junction of the right atrial appendage and the superior vena cava, and courses leftward across the interatrial groove to insert into the base of the left atrial appendage and the anterosuperior left atrial wall. The bundle is well-delineated and in most cases, a fine fatty layer is interposed between the underlying myocardium and the bundle.
This bundle contains predominantly longitudinally oriented myocardial fibers, aiding in fast passage of the electrical depolarization from the right atrium to the left atrium. This explains why, under normal conditions, the left atrium contracts only milliseconds after the right atrium. Bachmann's bundle is one of the components of the cardiac conduction system, and forms part of the specialized bundles of myocardial tissue that take the electrical impulses from the sinoatrial node to the atrioventricular node and the left atrium,
When Bachmann’s bundle is intact, left atrial activation is almost simultaneous with the right atrium. If it is damaged, it can cause varying degrees of interatrial block (IAB), and electrical conduction must proceed through other less effective pathways, resulting in atrial dyssynchrony and altered cardiac rhythm. Advanced IAB is strongly associated with atrial fibrillation, left atrial mechanical dysfunction, and increased risk of stroke even in sinus rhythm.
IAB can be caused by fibrosis, fatty infiltration, atrial dilation, aging, ischemia, and iatrogenic damage in prior cardiac surgery or ablation. All these preferentially affect the anterosuperior interatrial region, explaining the bundle’s vulnerability.
There are anatomical variations of Bachmann's bundle. In some cases, the bundle is separated from the atrial wall by epicardial fat, and in some cases it hugs the surface of the atria. In this last instance the bundle is more susceptible to damage by internal ablation in the left atrial wall. The location of the bundle can also vary.
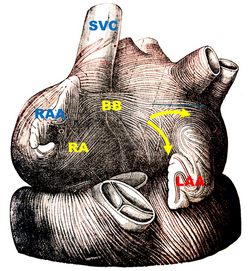
Bachmann’s bundle shows some bifurcations, helping to distribute the depolarization to the left atrium. The image, from Testut & Latarjet (1931), shows one of these bifurcations (yellow arrows). The bundle splits around the base of the left atrial appendage (LAA).
Historically, all pacemakers terminal wires have been implanted in the right atrium. but the potential dysfunction of Bachmann's bundle would require biatrial pacing, which is not used today.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. Antonio Bayés de Luna, Albert Massó-van Roessel, Luis Alberto Escobar Robledo, The Diagnosis and Clinical Implications of Interatrial Block, European Cardiology Review 2015;10(1):54–9
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. "Tratado de Anatomia Humana" Testut et Latarjet 8th Ed. 1931 Salvat Editores, Spain
8. 4. Rigamonti F, Shah DC. "Bachmann Bundle Block Occurring During Radiofrequency Ablation at the Inter-Atrial Septum" J Clin Med. 2012;15(9):263.
9. Zhang Y, Wu F, Gao Y, Wu N, Yang G, Li M, Zhou L, Xu D, Chen M. "Bachmann bundle impairment following linear ablation of left anterior wall: impact on left atrial function". Int J Cardiovasc Imaging. 2022 Jan;38(1):41-50
10. Platonov, PG; Mitrofanova, L, et al.Substrates for intra-atrial and interatrial conduction in the atrial septum: Anatomical study on 84 human hearts Heart Rhythm,(2008)5:8,1189-1195.
- Details
- Written by: Efrain A. Miranda, Ph.D.
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.
Jean George Bachmann (1877–1959) was a French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Sir Arthur Keith and Martin W. Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
- Details
- Written by: Efrain A. Miranda, Ph.D.
Homeostasis is the coordinated set of physiological mechanisms that preserve a stable internal bodily environment (through feedback-controlled regulatory processes) despite fluctuations in the external environment. The concept applies to many dynamic regulations of physiological variables such as body temperature, pH, electrolyte balance, osmolarity, blood glucose, etc.
Claude Bernard (1813–1878) introduced the concept of a “milieu intérieur” the “internal environment” in 1865 where he stated “La fixité du milieu intérieur est la condition de la vie libre et indépendante.” (The constancy of the internal environment is the condition for a free and independent life). Walter B. Cannon (1871–1945) formally coined the term homeostasis in 1929. In his reasoning to name these processes under one name he used the Greek term "ομοιόσταση" [omeóstasí) meaning "constant & stable" or "similar & standing still" referring to a constant (internal) environment.
Disruption of homeostatic processes can contribute to disease states such as diabetes mellitus (failure of glucose homeostasis), heart failure (impaired circulatory stability), heat stroke and/or hypothermia (thermoregulatory failure), hyponatremia or hypernatremia (electrolyte imbalance), etc.
For additional information here is an article from the National Library of Medicine.
Sources:
1. Claude Bernard, "Introduction à l’étude de la médecine expérimentale" (1865).
2. “Organization for physiological homeostasis” Cannon W. B.; Physiol Rev. 1929; 9:399–431.
3. "Textbook of Medical Physiology"; Guyton, Arthur C and Hall, John E ISBN: 0721659446 USA: W.B. Saunders, 1996.
4. “Homeostasis and Body Fluid Regulation: An End Note”. De Luca LA Jr, David RB, Menani JV. Neurobiology of Body Fluid Homeostasis: Transduction and Integration. Boca Raton (FL): CRC Press/Taylor & Francis; 2014. Chapter 15
- Details
- Written by: Efrain A. Miranda, Ph.D.
One of the problems with the concept of the ganglionated plexuses (also known as ganglionated plexi or GPs) is that these structures are rarely mentioned in medical education and are known only to specialists. People looking for information on this topic rarely find a detailed explanation. This article’s objective is to explain these structures and their function, as well as include some historical vignettes. We will start with a review of the structure and organization of the human nervous system.
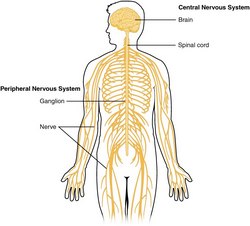
The nervous system is a complex network responsible for coordinating bodily functions and maintaining homeostasis, that is, to maintain a constant internal environment despite a variable external environment. It operates as the body’s control center, enabling interaction between different parts of the body and facilitating interactions with the environment, both external and internal. It is composed of two main types of cells: neurons and neuroglia, also known as glial cells. Neurons are responsible for transmitting information through electrical and chemical signals. Glial cells support and protect neurons, also helping in their nutrition.
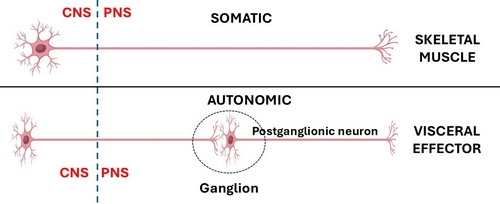
The nervous system is divided into a central nervous system (CNS) and a peripheral nervous system (PNS). The CNS is that portion (brain and spinal cord) contained within the craniospinal cavity and the PNS is composed of neurons and nerves outside this cavity.
It must be noted that these divisions of the nervous system are didactic, that is, they have been created to teach and understand its organization. The fact is that humans have only one nervous system.
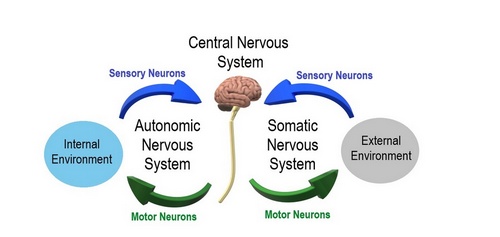
Another division of the nervous system is that of a somatic component and an autonomic component. The somatic component controls voluntary movements and conveys sensory information to the CNS. The autonomic nervous system (ANS) manages involuntary functions such as heartbeat, digestion, urination, etc. For this article we will focus on the ANS.
The ANS is further divided into a sympathetic division, which prepares the body for stress or emergencies (fight or flight response); and a parasympathetic division, which conserves energy, slows down the body and restores the body to a state of calmness (rest and relaxation). Within the ANS we will find motor (efferent) and sensory (afferent) neurons.
Within the PNS and as part of the ANS there are accumulations of neuronal bodies within or close to the internal organs of the body. Each one of these is called a ganglion (Pl. ganglia). The most recognized ganglia are those that compose the sympathetic chain and those related to the origin of most of the branches of the abdominal aorta (Superior mesenteric, celiac, renal, inferior mesenteric, etc.)
In the case of the CNS somatic (bodily, voluntary) motor organization, is composed of one neuron that is usually located in the frontal lobe motor cortex of the brain in the area known as the precentral gyrus. The distal motor effector of these neurons are distributed to striated (voluntary) muscles throughout the body.
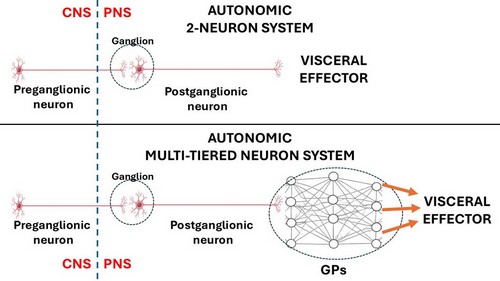
The ANS has been classically described as a 2- neuron system. The body of the first one is found in the CNS and is called the preganglionic neuron, the body of the second one is found in a PNS ganglion and is called the postganglionic neuron, which connects to an autonomic effector (smooth muscle or glands). John Newport Langley (1852 – 1925) a British physiologist coined the terms “preganglionic” and “postganglionic”.
This classic 2-neuron description works for glands and some organs, but it does not consider organs that have rhythmic activity, such as the digestive system and its peristalsis, the heart, ureters, etc.
AI generated image of a neural network
The rhythmicity of these organs is so complex that it requires additional neurons within the muscle layers of each organ. These neurons are found in small intramural ganglia which interconnect with other ganglia by way of nerve fibers forming a complex meshwork (Lat: Plexus). These are the ganglionated plexi (GPs) and their function is to reduce the workload of the CNS by working mostly on their own with oversight of the CNS. These GPs have multiple interconnections forming a neural network, quite similar (on a smaller scale) to the organization of the brain.
Thus, the ANS should be considered as a 2- neuron system in cases such as glands and some organs but, in the case of rhythmic organs there will be ganglionated plexi between the postganglionic neuron and the effector, making it a multiple-tiered system depending on the number of neurons that are interconnected within the GPs.
The two most well-known ganglionated plexi are those found in the muscular and submucosal layers of the small intestine. These plexuses are also found in all the digestive system organs but are more easily studied in the small intestine. They are the plexus of Meissner (submucosal) and the plexus of Auerbach (myenteric). Together they control peristalsis, regulate local secretion and absorption, and modulate blood flow. These nerve plexuses were first described by Leopold Auerbach (1828 -1897) in 1857 and Georg Meissner (1829 – 1905) in 1864.
Because of the importance of these GPs and their activity, they have been called the “enteric nervous system” or the “little brain of the gut” by scientists and journalists. In my opinion, this moniker isolates these GPs from their function as part of the whole of the nervous system.
Another organ that has the same two-layered GPs is the ureter, as described by Pieretti (2018). Neurons (GPs) have been found in the walls of the urethra.
There are organs that have both voluntary and involuntary innervation, such as the urethra, urinary bladder, parts of the anal sphincters, etc. An interesting example of this is the respiratory diaphragm. Most of the day, we are not aware of it working (involuntary – ANS dependent), but if you want to, you can take a deep breath at will (voluntary – somatic dependent)
GPs have been described in the heart, which is a quintessential rhythmic organ. Our life depends on its rhythmicity which helps pump blood through the body. Even before the GPs were discovered, the innervation of the heart was described in detail by Antonio Scarpa (1752 – 1832) in his book “Tabulæ Neurologicæ” published in 1794.
The first to describe GPs in the heart was Robert Remak (1815 – 1865) in 1838, they were known as ”Remak’s ganglia”. Later studies were carried out by Woolard (1926), Singh (1996), Pauza (2000), and others. In these research papers great images of the neuron component of these GPs were published.
Before continuing with the topic of the GPs it is necessary to divert slightly to discuss the conduction system of the heart. The conduction system of heart has been described as a group of nodes and fibers that carry electrical impulses within the heart. (sinoatrial node, interatrial and atrioventricular bundles, atrioventricular node, bundle branches, Purkinje fibers). What is not commonly known is that this system is not formed by neurons and nerves, but by specialized cardiomyocytes (heart muscle cells). Each one of these specialized cells has an automaticity that allows them to beat at a specific number of beats per minute (bpm). The further distally within the conduction system the slower the bpm of each of these muscle cells.
So, if each muscle cell has a predetermined bpm count, how does the heart rhythm increase or decrease when needed? The answer lies in complex reflexes mediated by the GPs and in the interaction of the ANS with the GPs of the heart.
The GPs and their interconnections form the intrinsic cardiac nervous system (ICNS), which has several important functions:
Heart Rate Regulation: The GPs modulate the activity of the sinoatrial (SA) node, which is responsible for initiating the heartbeat.
Conduction Modulation: The GPs also modulate the conduction pathways in the heart, particularly the atrioventricular (AV) node and Purkinje fibers, ensuring coordinated contractions of the heart muscle.
Cardioprotection: The GPs help protect the heart by altering cardiac output in response to exercise, stress, ischemia, etc., maintaining heart function and helping homeostasis under challenging conditions.
Coordinate Local Reflexes: The GPs integrate sensory information from the heart and coordinate local reflexes, allowing for rapid adjustments to changes in the heart's environment.
These functions highlight the importance of ganglionated plexuses in maintaining heart health and responding to physiological demands. Dysfunction in these plexuses can lead to various cardiac issues, including arrhythmias, particularly atrial fibrillation (AFib), and heart failure.
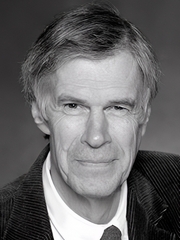
J. Andrew Armour
Cardiac GPs are found in the cardiac wall, although most of them are found intramural and superficial (epicardially) (Tan, 2006), and also embedded in epicardial fat, in the areas devoid of pericardium (formed by the pericardial reflections) around the pulmonary veins, superior vena cava and around the ligament of Marshall. Although GPs are found in the atria and ventricles, there are 5 times more atrial than ventricular GPs (Armour, 1997).
In the study of the GPs, J. Andrew Armour MD, PhD, has been a foundational figure in neurocardiology, and his work has shaped our modern understanding of the intrinsic cardiac nervous system (ICNS), and the GPs. He proposed that the ICNS is not just a passive relay for ANS signals, but a complex integrative network of efferent (motor) neurons, afferent (sensory) neurons, and local circuit neurons that form the GPs. Through his work, Armour argued that the heart’s neuronal network is sufficiently rich to process information, participate in local reflexes, and modulate cardiac function independent of central nervous system input. This can be proven by the heart working normally in heart transplants, completely separated from the recipient's nervous system.
In conclusion, there are two points to consider:
1. The 2-neuron organization of the ANS must be expanded to consider all organs that have rhythmicity and have GPs forming an intramural neural network, following this schema.
2. Our understanding of the rhythmicity of the heart has been one-sided, focusing only on the cardiomyocyte-based conduction system of the heart. This leads to surgical and minimally invasive treatments that do not consider the ICNS and GPs, as well as the location of most of the GPs on the external layers of the heart. A unified approach to these structures will certainly help those patients with cardiac arrhythmias and their surgical treatment.
Sources:
1. Stavrakis S, Po SS. “Ganglionated Plexi Ablation: Physiology and Clinical Concepts.” Heart Rhythm 2017. Arrhythm Electrophysiol Rev 6(4):186–190
2. “The Intrinsic Cardiac Nervous System and Its Role in Cardiac Function” Fedele L, et al. 2020. J Cardiovasc Dev Dis 7(4):54.
3. "A brain within the heart: A review on the intracardiac nervous system" Campos, I.D.; Pinto, V.J Mol and Cell Cardiol. 2018 119:1-9
4. "Anatomical Distribution of Ectopy-Triggering Plexuses in Patients with Atrial Fibrillation" Kim, MY et al Circulation" Arrythmia and Electrophysiol 2020. 13:9
5. “Morphology, Distribution, and Variability of the Epicardiac Neural Ganglionated Subplexuses in the Human Heart” Pauza, D., Skripka, V et al The Anatomical Record 259:353–382 (2000)
6. “Gross and Microscopic Anatomy of the Human Intrinsic Cardiac Nervous System” Armour JA et al, (1997) The Anatomical Record 247:289-298
7. “The Junction Between the Left Atrium and the Pulmonary Veins, An Anatomic Study of Human Hearts” Nathan, H; Eliakim, M. Circulation (1966) 34: 412-422
8. “Autonomic innervation and segmental muscular disconnections at the human pulmonary vein-atrial junction: implications for catheter ablation of atrial-pulmonary vein junction” Tan AY, Li H, Wachsmann-Hogiu S, Chen LS, et al J Am Coll Cardiol 2006;48:132–143
9. “Topography of cardiac ganglia in the adult human heart” Singh S, Johnson PI, Lee RE, Orfei E, Lonchyna VA, Sullivan HJ, et al. J Thorac Cardiovasc Surg 1996; 112:943-53
10. Woollard, H. H. “The Innervation of the Heart.” Journal of anatomy (1926) 60 Pt 4: 345-73. 4
11 “Tabulæ Neurologicæ ad illustrandam historiam anatomicam cardiacorum nervorum, noni nervorum cerebri, glossopharyngæi, et pharyngæi ex octavo cerebri. ” Scarpa, A. 1794 Balthasarem Comini Pub.
12.“The Involuntary Nervous System” Gaskell, W. H.2nd Ed. Longman, Green & Co. 1920
13. “Cardiac anatomy pertinent to the catheter and surgical treatment of atrial fibrillation”. Cox. JL et al J Cardiovasc Electrophysiol 2020 Aug;31(8):2118-2127. doi: 10.1111/jce.14440.
14. "Minimally Invasive Surgical Treatment of Atrial Fibrillation: A New Look at an Old Problem" Randall K. Wolf, Efrain A. Miranda, Operative Techniques in Thoracic and Cardiovascular Surgery, 2024,
15. “Correlative Anatomy for the Electrophysiologist: Ablation for Atrial Fibrillation. Part I: Pulmonary Vein Ostia, Superior Vena Cava, Vein of Marshall” Macedo PG, Kapa S, Mears JA, Fratianni A, Asirvatham SJ. J Cardiovasc Electrophysiol. 2010 Jun 1;21(6):721-30.
16. “Treatment of lone atrial fibrillation: minimally invasive pulmonary vein isolation, partial cardiac denervation and excision of the left atrial appendage” Wolf, R.K. Ann Cardiothoracic Surg. 2014; 3:98-104
17. “Neurocardiology: Anatomical and Functional Principles” Armour, J.A. Institute of HeartMath, Boulder Creek, CA, 2003
18. “The enteric nervous system: a little brain in the gut" Annahazi, A. ∙ Schemann, M. Neuroforum. 2020; 26:31-42
19. “The Little Brain Inside the Heart” Dr. José Manuel Revuelta Soba Professor of Surgery. Professor Emeritus, University of Cantabria, Spain
Images
Image of the CNS - Public Domain. Source: WikipediaCreative CommonsAttribution 4.0 International license.
Autonomic and Somatic Image. Public Domain by Christine Miller. Source: WikipediaCreative CommonsAttribution 4.0 International license.