Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 1301 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
- Written by: Efrain A. Miranda, Ph.D.
Peripheral nerve injuries can result from trauma, compression, thermal damage or systemic diseases, and their classification is essential for diagnosis, management, and prognosis. Three key terms are used to describe the severity and nature of these injuries: neurapraxia, axonotmesis, and neurotmesis. They describe the structural and functional integrity of nerve fibers after injury. The etymology of these terms derives from the Greek language.
These terms were initially proposed by Sir Herbert John Seddon (1903 – 1977), an English anatomist and orthopedic surgeon who published his initial findings in 1943, followed by Sir Sydney Sunderland (1910 – 1993), an Australian orthopedic surgeon who published a revised classification in 1951. The terms coined by Seddon and Sunderland and their classification system into 5 Grades of Nerve Injury remain central to the treatment of nerve injuries today.
Neurapraxia:
Neurapraxia represents the mildest form of nerve injury. It is characterized by a temporary block of nerve conduction without axonal disruption. Recovery is typically complete and occurs within days to weeks.
• No structural damage to the axon or surrounding connective tissue.
• Localized demyelination may occur, leading to a conduction block.
• Commonly results from compression or mild blunt trauma (e.g., “Saturday night palsy” or a "transient ulnar nerve palsy").
The term is derived from the Greek [νεῦρον] meaning “nerve” and [πρᾶξις] (praxis) meaning “action”. In medical terminology “a” or “an” means “without” or “absence of”. Thus, the word is constructed as [neur]-[a]-[praxia] meaning “absence of nerve function”.
Axonotmesis
Axonotmesis is a more severe injury in which the axon is damaged, but the surrounding connective tissue structures (endoneurium, perineurium, and epineurium) remain intact. Wallerian degeneration occurs distal to the lesion, and axonal regeneration following the intact connective tissue channels can allow for not only nerve regeneration but regain of function of the damaged nerve. This is the mechanism of action of cryoneurolysis devices used in surgery.
• Axonal continuity is lost, but the scaffolding remains.
• Regeneration can occur at a rate of approximately 1–3 mm/day.
• Often seen in crush injuries or prolonged compression.
The term is derived from the Greek [ἄξων] meaning “axis” and [τμῆσις], meaning “division” or “cut”. Axonotmesis means “division (cutting) of the axon.”

Augustus Volney Waller (1816 – 1870)
Neurotmesis
Neurotmesis is the most severe form of nerve injury. It involves complete disruption of the axon and surrounding connective tissue, as would happen when a nerve is transected or avulsed. It results in permanent loss of function, since when the axons start to regrow, there are no connective tissue “tunnels” to guide the growing axon to their terminal connections. One of the problems that may happen is the formation of a neuroma or neurinoma at the site of nerve transection.
The only way to attempt to restore function is with surgical intervention bringing the cut ends of the nerves together, sometimes using microsurgery. The results of surgery are not always optimal
• Wallerian degeneration occurs distal to the injury.
• Regeneration is not possible without surgical repair.
• Typically is the result from lacerations, severe traction injuries, or penetrating trauma.
The term is derived from the Greek [νεῦρον] meaning “nerve” and [τμῆσις] meaning “division” or “cut”. Neurotmesis thus translates to “division of the nerve.”
Accurate classification of nerve injuries can help guide prognosis and treatment:
• Neurapraxia: Managed conservatively with physical therapy and observation.
• Axonotmesis: May require surgical exploration if function does not return within expected time frames.
• Neurotmesis: Early surgical intervention is usually necessary to restore any function.

Note: The term “Wallerian degeneration” is associated eponymically with Augustus Volney Waller (1816 – 1870), an English physiologists know for his work on nerve injury and regeneration.
Personal note: Most people talk about "peripheral nerves", as if "central nerves" existed. This is not so. Within the Central Nervous System (CNS) the bundles of axons have different names such as "fascicles" (fasciculus lenticularis), tracts" (spinothalamic tract), lemniscus (medial lemniscus), etc. These central bundles of axons form structures that themselves have separate names, such as the corpus callosum, internal capsule, external capsule, anterior commissure, etc. All of these structures lack a well formed connective tissue wrap, which is the reason why transection of these structures usually does not allow recovery, such as in the case of spinal cord transection.
Nerves, which are only found in the Peripheral Nervous System (PNS). do have a well-formed connective tissue wrap formed by the endoneurium, perineurium, and epineurium. The presence of these connective tissue structures is what allows for nerve regeneration and recuperation of functionality.
To be precise then, using the term "peripheral nerve" is redundant, as all nerves are peripheral! Dr. Miranda
Sources
1. Seddon H. Three Types of Nerve Injury. Brain. 1943;66(4):237-88. doi:10.1093/brain/66.4.237
2. Seddon H, Medawar P, Smith H. Rate of Regeneration of Peripheral Nerves in Man. J Physiol. 1943;102(2):191-215. doi:10.1113/jphysiol.1943.sp004027
3. Sunderland S. A Classification of Peripheral Nerve Injuries Producing Loss of Function. Brain. 1951;74(4):491-516. doi:10.1093/brain/74.4.491
4. O'Brien, M. D., & Wade, D. T. (1992). Neurological rehabilitation. Chapman and Hall.
5. Liddell, H. G., & Scott, R. (1940). A Greek-English Lexicon. Oxford University Press.
6. "The Origin of Medical Terms" Skinner 1970
7. "Dorland's Illustrated Medical Dictionary" 28th Ed. W.B. Saunders. 1994
8. “Stedman’s medical eponyms” Farbis, P; Bartolucci, S. Williams & Wilkins 1998
9. https://radiopaedia.org/articles/sunderland-classification-of-nerve-injury
10. " Correlative Neuroanatomy and Functional Neurology" Chusid, Joseph. Lange Medical Publications
The image of H.J. Seddon is an AI composite of the few images and portraits available. Courtesy OpenAI.
- Details
- Written by: Efrain A. Miranda, Ph.D.

G.E. Rindfleisch (1836 – 1908)
This article is an anatomical, physiological, and terminological discussion for two related cardiac structures: The Vincula Aortæ and the cardiac folds of Rindfleisch.
The topic of this article was triggered by a LinkedIn post by Dr. Guillermo Stöger, an Argentinian cardiac surgeon who works in the Cardiac Department of the Heart Center in Leipzig, Germany.
In his post, Dr. Stöger describes the Vincula Aortæ as “communication or adhesions” between the intrapericardial portion of the ascending aorta and the intrapericardial portion of the pulmonary trunk. In this segment these two vessels share their adventitia layer as well as a rich vascular supply. Dr. Stöger also describes the presence of small vessels in the area, which can cause a hematoma when a dissection or trauma of one of this vessels happens.
So, what is the Vincula Aortæ? It was first described by Georg Eduard Von Rindfleisch (1836-1902), a German pathologist and histologist in an article in German published in 1884 titled “Ligament-like connections between the aorta and pulmonary artery (vincula aortae)” [1]. In this article Rindfleisch describes the movement of the pulmonary trunk and ascending aorta caused by the pressure fluctuations between systole and diastole, forcing these two structures to twist and separate in opposite directions. While the ascending aorta tends to move towards the right sternoclavicular joint, the pulmonary trunk tends to move towards the left third intercostal space. Rindfleisch states that the presence of the intervascular “ligaments” reduces the mobility of these structures.
Being a histologist, Rindfleisch describes the structure of this intervascular structure (the Vincula Aortæ) as containing connective and fibrofatty tissue with vascular structures, encased in adventitia, and all of them covered by the visceral pericardium (endocardium). The accompanying image, modified from the original by WC Roberts [12], shows how the ascending aorta and pulmonary trunk share their adventitia; the arrows point to the area where there is connective tissue. Rindfleisch posits that the constant movement of the vessels and pericardium slowly causes the pericardium to wrinkle and fill with fat causing a semilunar elevation 2 -3 cm superior to the root of the aorta. He says that these fatty pads are more evident in people over 40 years of age.
It should be pointed out that Rindfleisch described the intervascular communication between the ascending aorta and pulmonary trunk, as a “clamp”, and also as “adhesions” or “ligaments”, and he named them “Vincula Aortæ”; but although he described the pericardial fatty fold caused by the movement of these structures, he did not name it. Later they were eponymically referred to as the “folds of Rindfleisch”. According to Netter [2] when more than one is present only the larger and usually most superior of these folds is so called.
The following mage is from Rindfleisch’s 1884 article and shows a tear in the ascending aorta with an aortic dissection. Interestingly, he says that the tears in the aorta (or pulmonary trunk) happen higher in these vessels, distal to the Vincula Aortae, which gives the lower segments additional strength.
In 2003 Morrison et al [3] published a description of the Fold of Rindfleisch stating that they were “unaware of a formal description of this structure”, naming it “crista aortæ ascendentis”. They described neurovascular bundles, fat and connective tissue in this structure, ending with a recommendation to do careful hemostasis to avoid hemorrhage intra and postoperatively, just as Dr. Stöger suggested recently.
In a “Letter to the Editor” following Morrison’s publication, Dr. Wesley Parke refuted it stating that the structure in question had already been described 40 years earlier in 1966 by himself [4], followed by a detailed study of the vessels in the region in 1970 [5]. Parke references brief statements on these folds by Davis in 1927 [6] and Hans Smetana in 1930 [7]. Parke calls this fold the “aortic ridge” and ascribes to it a cushioning function between the aorta and the right atrial appendage. No mention of Rindfleisch.
The image (modified from Parke's 1966 original) shows two specimens of the ascending aorta. The arrows point to the folds of Rindfleisch. Note that specimen 3 has a double semilunar fold.
The importance of the work of Dr. Wesley Parke is the detailed description of the “vasa vasorum” that provide blood supply to the aorta and pulmonary trunk creating a plexus of vessels. Careful hemostasis is needed to prevent bleeding when working at the root of the pulmonary trunk and aorta.
Parke mentions Hans Smetana (1894 - 1977). His paper "Vasa Nutritia der Aorta" describes the many vasa vasorum of the aorta and his work was followed by W. Parke who described the complex blood supply to the ascending aorta and pulmonary trunk. Following are two images modified from the original works by these authors. Again, it is critical to point out the importance of these vessels found in the area of the Vincula Aortae when performing surgery.
There are research articles on the fatty ridges found in the proximal ascending aorta, but many have forgotten the contributions of Rindfleisch. In 1999 F. Unger named it the “plica transversa aortæ” [8]. This letter was criticized, by Falkowski et al [8] reminding that the structure was first named “Plica semilunaris nach Rindfleisch” by Julius Tanders (1869 – 1936) in his book “Anatomie des Herzens” [10]. Falkowski says “it is not the first time we have encountered self-given names to structures that have been previously studied and named a century, and sometimes centuries ago”.
Rindfleisch was the first to describe and name the common connective tissue and adventitia between the intrapericardial ascending aorta and pulmonary trunks (vincula aortae) and the fold of pericardial tissue that should bear his name: the aortic semilunar fold (plica semilunaris aortæ) of Rindfleisch.
Sources:
1. “Uber Klammeratigae Verbindungen zwischen Aorta und Pulmonal arterie (Vincula aortae)”. Rindfleisch E Von. 1884. Virch Arch Pathol Anat Physiol Klin Med 96: 302–306.
2. “CIBA collection of medical illustrations” Netter F. 1971; vol 5, The Heart. section 1, plate 5.
3. “Surgically Relevant Structure on the Ascending Aorta” Morrison, JJ; Codispoti, M; Campanella, C. 2003 J Clin Anat 16:253-255
4. “The human aortic ridge and cushion” Parke, WW; Michels, NA 1966 Anat Rec, 154: 185-193.
5. “The vasa vasorum of the ascending aorta and pulmonary trunk and their coronary and extracardiac relationships” Parke WW. 1970 Am Heart J 80:802– 810
6. “The periaortic fat bodies” Davis DJ. Arch Path and Lab Med 1927 4:937-942
7. “Vasa Nutritia der Aorta: Smetana, H. 1929 Virchows Archiv für pathologische Anatomie und Physiologie und für klinische Medizin. 274: 170-187
8. “The Plica Transversa Aortae: An Addendum to the Anatomic Nomenclature of the Heart” Unger, F. 1999 Ann Thorac Surg 68:2383-91
9. “Plica transversae aortae—fold of Rindfleisch” Falkowski, G; Dzigivker, I; Bitran, D. 2001 Ann Thorac Surg 7:1-761-762
10. “Anatomie Des Herznes” Tandler, J et al. 1913. Publisher Gustav Fischer
11. “"Tratado De Anatomía Humana” Testut, L.; Latarjet, A. Barcelona, Spain: Salvat Editores, 1943.
12. “Aortic dissections: Anatomy, consequences, and causes” Roberts WC (1981). Am Heart J 101:195-214.
13 “The Fatty Ridge and Fatty Cushion of the Human Pulmonary Trunk” Nadkarni, SD, et al. Anatomical Record 1976 187: 107-112
14."Stedmans Medical Eponyms" Forbis, P.; Bartolucci, SL; 1998 Williams and Wilkins
- Details
- Written by: Prof. C. Uribe

The anatomical framework of the seven books
that comprise Vesalius' Fabrica
As an educator with over 20 years teaching Human Anatomy, I have witnessed how accurate and up-to-date language can transform teaching and learning in health sciences.
The recent publication of Anatomical Terminology 2 (TA2), made freely available by the International Federation of Anatomists' Associations (IFAA), represents a significant advance that all professionals in the field should adopt as soon as possible.
Anatomical terminology is not simply a list of terms, but the basis for clear, effective and universal communication. The TA2 update addresses not only necessary changes resulting from new anatomical research and discoveries, but also substantial improvements in consistency and accuracy. This is especially relevant today, when globalization and digitalization demand accurate communication between professionals from different countries and specialties.
Using TA2 involves:
- Unifying anatomical criteria globally.
- Facilitating the teaching of anatomy with clear and precise terms.
- Improving the quality and safety of healthcare by reducing misunderstandings.
- Empowering scientific research by ensuring consistency in academic publications.
I invite fellow teachers, students and health professionals to familiarize themselves with TA2 and actively apply it in their academic and clinical practices. Let us take advantage of this tool to continue raising the standard of our work and the quality of anatomy education.
You can consult TA2 directly at this link: https://libraries.dal.ca/Fipat/ta2.html
What has been your experience with the update of anatomical terminologies?... Are you ready to integrate TA2 into your teaching and professional practice?
- Details
- Written by: Efrain A. Miranda, Ph.D.
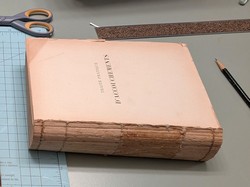
Recientemente recibí un libro de Chile. Este libro está en Francés y se titula “Traité D’Accouchements” (Tratado sobre el Parto) o “Tratado de Obstetricia”, y se publicó en 1898 en París. El autor es el Dr. Pierre-Victor Alfred Auvard (1844 - 1940), un Ginecólogo-obstetra Francés,
El libro pertenecía a la biblioteca del Hospital San José. El Antiguo Hospital San José es un exhospital ubicado en la calle San José, a un costado del Cementerio General de Santiago, en la comuna de Independencia, ciudad de Santiago, Chile. Construido entre los años 1841 y 1872 funcionó como hospital hasta 1999, cuando se construyó el nuevo Hospital San José.Este hospital ahora está siendo demolido y se construirá uno nuevo en su lugar, pero los libros viejos de la biblioteca fueron desechados sin contemplaciones.Un ingeniero a cargo de las nuevas obras logró rescatar algunos de estos libros y uno de ellos fue traído de Chile a Estados Unidos por otro amigo mío, Carlos Verdugo, compañero de colegio.
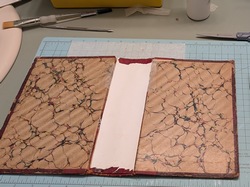
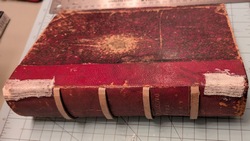
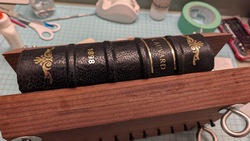
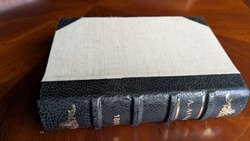
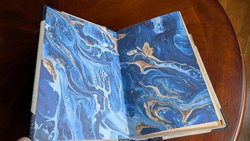
El libro estaba en pésimas condiciones, con un título apenas legible, el lomo roto y los folletos internos separados porque los hilos que lo sujetaban estaban rotos. Como la encuadernación y la reparación de libros son otra de mis aficiones, me encargué de la tarea y ahora se añadirá a mi colección. Aquí hay algunas fotos del proceso. Haga clic en la imagen para verla más grande.
En una de sus páginas, el libro tiene un sello antiguo y apenas legible que dice "Manuel Casanueva del C". Una breve búsqueda indicó que se trataba del sello Ex-Libris del cirujano chileno Dr. Manuel Casanueva del Canto. Por supuesto, tuve que investigar un poco sobre el antiguo propietario de este libro.
Manuel Casanueva del Canto nació en la ciudad de Linares, Chile, el 5 de julio de 1908. De 1925 a 1931 cursó del primero al sexto año de medicina en la Facultad de Medicina de la Universidad de Chile (donde yo estudié). En ese entonces, la Facultad de Medicina estaba en el barrio Independencia de Santiago. En 1930 obtuvo su licenciatura en medicina.

El libro reparado en mi biblioteca
Entre 1930 y 1931 fue residente de cirugía en el Hospital San Francisco de Borja (donde fue paciente de niño), pasando por Medicina Interna, Medicina de Urgencias y Cirugía y Obstetricia, obteniendo su título de cirujano en mayo de 1932. Su tesis de grado se tituló “Anatomía Patológica: Alteraciones inflamatorias de la vesícula biliar”.
Como cirujano, trabajó en el Hospital Militar de Santiago, el Servicio Central de Urgencias y el Hospital Central de Traumatología. En 1952, volviendo a sus orígenes, se trasladó al Departamento de Cirugía de la Universidad de Chile, en el Hospital José Joaquín Aguirre. Este hospital se encuentra en el mismo campus que la Facultad de Medicina donde estudió.
En 1955 postuló (y obtuvo) el puesto de Profesor Extraordinario de Cirugía Patológica en la Facultad de Medicina de la Universidad de Chile. Para entonces, ya contaba con una destacada trayectoria docente, varios premios médicos, y fue autor del libro "Transfusión Sanguínea Práctica" en 1939, además de ser coautor de varios libros médicos y más de 81 artículos.
Se convirtió en Jefe de Cirugía del Hospital José Joaquín Aguirre y en 1961 invitó a Pablo Neruda, chileno ganador del Premio Nobel de Literatura, a impartir una conferencia en el hospital.
En 1975, la Editorial Andrés Bello publicó su libro "Cirugía", en dos volúmenes en español. No he podido encontrar este libro. No se sabe mucho de él después de esta fecha. No se ha encontrado ninguna fotografía ni retrato.
Se casó con María Yolanda Carrasco Coral (fecha desconocida) y tuvieron tres hijos: María Cristina, Isabel y Manuel Luis.
Falleció el 13 de febrero de 1981 en Viña del Mar y está enterrado en Santiago de Chile. Investigaciones posteriores indicaron que este libro que recibí de regalo fue donado a la biblioteca del Hospital San José por el Dr. Casanueva, donde finalmente fue desechado, rescatado, transportado a Estados Unidos y reparado.
Espero que este artículo llegue a la los descendientes de la familia Casanueva del Canto en Linares (hoy son Casanueva Carrasco y/o Casanueva Iommi) y que me ayuden a actualizar esta investigación y tal vez obtener una foto del Dr. Casanueva del Canto. El artículo original en Inglés puede leerse aquí.
- Details
Personal Note: A few weeks ago, I came across a very interesting article in Spanish by Dr. Jose Manuel Revuelta from the University of Cantabria, Spain. The article (in Spanish) talked about the “small brain inside the heart”. One of my interests in the anatomy of the heart is the intrinsic system called the cardiac “ganglionated plexuses”, “ganglionated plexi”, or “GPs”.
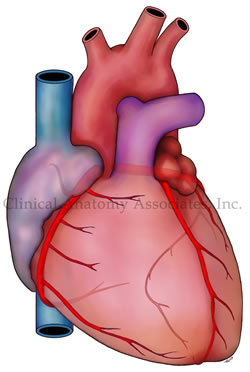
It is our proposal that this nervous system inside the heart, which works autonomously (if needed to or forced to) and also dependent, of the autonomic nervous system, is responsible for the intrinsic working of the heart and its dysfunction is probably the root of cardiac dysrhythmias. We have several seminars on this topic here.
In a recent publication with Dr. Randall K. Wolf, we explained both the Wolf Procedure and the anatomical basis that underline atrial fibrillation.
The concept of the "small brain of the heart" is not new. It has been mentioned by Woolard (1926), Armour (1997), Pauza (2000), and others. These authors and others are referenced in this publication. Unfortunately, the diffusion of the concept of an intrinsic, interconnected mesh of clusters of neurons within the heart and other organs that have rhythmic activity, has many names used by the media. That is why you can find articles on the "little brain of the gut", the "gut brain", the "enteric nervous system", the "little brain of the heart", etc.
Dr. Revuelta's article shows that the interest on the GPs continues on, and more research is being done on this topic. He has graciously granted us permission to translate and publish his article in “Medical Terminology Daily”. He has also expressed interest in publishing some of his articles in this blog. Dr. Miranda
The “Little Brain” Inside the Heart
Dr. José Manuel Revuelta Soba
Professor of Surgery. Professor Emeritus, University of Cantabria, Spain
In December 2024, the prestigious journal Nature Communications published that a group of researchers from the Karolinska Institute (Sweden) and Columbia University (United States) have discovered that the heart contains a small autonomous brain.
In general, scientific knowledge has been relating cardiac activity to the brain, as the only organ that regulates its functioning. This intimate bidirectional relationship regulates the adaptation of its rhythm and contractile force to changing energy demands, through impulses and signals transmitted by the autonomic nervous system. However, the heart surprises us again with new properties that go beyond what is known.
Autonomic nervous system
The neurovegetative nervous system of the human being is involuntary, comprising the sympathetic and parasympathetic nervous systems, essential for the functioning of the organism. They act in conjunction with the enteric nervous system, which also has involuntary action and regulates the activity of the gastrointestinal tract. The complex interactions between these autonomous systems, which have opposing actions, maintain cardiovascular homeostasis, that is, they provide the appropriate amount of oxygenated blood to the organs and tissues according to their demands.
The sympathetic nervous system regulates, among other functions, the body's response to any danger perceived as a threat to physical or mental health, known as the "fight or flight" reaction, described in 1915 by the physiologist Walter B. Cannon in the United States. This instinctive reaction leads to the immediate release of certain chemical substances into the blood, such as adrenaline and noradrenaline. These hormones act as neurotransmitters that produce an increase in the contractile force of the heart, tachycardia, contraction of blood vessels, hypertension and dilation of the airways. These neurotransmitters are released in the brain, facilitating the diffusion of their messages through the extensive network that forms this autonomous nervous system, increasing the state of alertness and eliminating any feeling of drowsiness. By producing an immediate tachycardia, it improves the supply of oxygen to the organs and tissues, enlarges the pupils and reduces the digestion of food to save energy and make it available for this reaction to an unexpected danger.
The parasympathetic nervous system controls the relaxation of the body at the end of the stress caused by the sudden “fight or flight” reaction, once the threat has passed, restoring the normal functioning of the organism. Its main function is the conservation and storage of energy through the release of acetylcholine, a powerful neurotransmitter, discovered by the English physiologist Henry H. Dale, for which he was awarded the Nobel Prize in Medicine in 1936. This substance produces vasodilation, reduction of blood pressure, decreased heart rate and increased intestinal motility.
The enteric nervous system has the exclusive mission of regulating the functioning of the gastrointestinal tract, which is completely covered by hundreds of millions of nerve fibers that transmit brain messages for digestive mobility and function, modifying the volume of blood flow via vasoconstriction or vasodilation.
The small brain of the heart
The innervation of the heart is more complex than previously thought, conditioned by messages from the autonomic nervous system and others from the organ itself. In the early 1990s, scientists described that the heart contained some neurons similar to those in the human brain, which led to speculation about the possible existence of independent neuronal activity within the heart that mediated its functioning and rhythm. This fascinating discovery soon became a priority objective of scientific research.
In 2021, James S. Schwaber and R. Vadigepalli, researchers at Thomas Jefferson University in Philadelphia, performed a three-dimensional mapping of the heart's neural center. They found that the heart receives constant information from the brain about the internal and external state of its environment, adjusting heart rate, blood pressure, and cardiac output. However, these messages also came from the heart's own neural system, called the "little brain," behaving as if there were an internal loop, something similar to what systems engineers call a programmable logic controller or PLC. Most of these neurons are located near the aortic and pulmonary valves, with their largest neuronal cluster (74 percent) located in the area of the sinoatrial plexus, on the upper lateral wall of the right atrium, in immediate relation to the mouth of the superior vena cava.
Using mathematical models, they observed that when this peculiar neural programmable logic controller was activated, it perfectly adjusted the heart's response to the various impulses and signals from the brain to improve cardiac performance, making its work more efficient. Without the presence of this "little brain" it would be impossible to eliminate or correct the possible errors and damage contained in some brain messages, so the heart could become erratic, causing irregular heartbeats or arrhythmias, as well as defects in its contractility.
As these scientists analyze their 3D heart models, obtained from various mammals, new questions arise about the actions of this "brain of the heart", its internal organization, its influence on the contractile force and rhythm of the heart, as well as its coordination and responses to the constant messages from the brain. Currently, these three-dimensional maps are being used to better understand how the vagus nerve connects with cardiac neurons, opening new opportunities for the greater integration of systems engineering into the field of cardiology.
Recent findings from the Karolinska Institutet and Columbia University have revealed that the heart does indeed have its own “mini-brain,” containing a nervous system that self-regulates its rhythm and function according to demand. This complex neurological center is made up of various types of neurons with different functions, some of which function as cardiac pacemakers.
This important research project was carried out in the zebrafish, an animal model that has great similarities with the human heart, both in terms of its heart rate and its general functioning. These scientists mapped the composition, organization and functions of neurons within this small intracardiac brain, using a combination of anatomical methods, electrophysiological techniques and neuronal RNA sequencing. They carried out a complete molecular and functional classification of intracardiac neurons, revealing a complex neuronal diversity within the heart itself.
This intracardiac neurological center is not part of the autonomic nervous system governed by the brain, contrary to what was believed. The data obtained in this interesting scientific investigation show that this “small brain” is made up of several types of independent sensory neurons with clear neurochemical and functional diversity. This population of neuronal cells allows the expression of various genes that encode various neurotransmitter receptors (glycine, glutamate, adrenergic, inotropic, GABA, muscarinic, serotonergic receptors, etc.), suggesting a complex network of neurotransmission specific to the heart, which ignores its total dependence on central orders from the brain.
“We were surprised to see the complexity of this small brain inside the heart, which has a key role in maintaining and controlling the heartbeat, similar to how the brain regulates other rhythmic functions such as locomotion and breathing. Better understanding this nervous system could lead to new insights into heart disease and help develop new treatments, such as for arrhythmias. We will continue to investigate how the heart’s brain interacts with the real brain to regulate cardiac functions under different conditions, such as exercise, stress or disease”, explains Konstantinos Ampatzis, a senior researcher at the Department of Neuroscience at Karolinska Institutet, Sweden, who led the study.
Future electrophysiological, pharmacological and molecular research will be critical to better understand the tangled interactions and complex regulatory mechanisms of the internal neurotransmission of this autonomous “small brain” and thus understand its overall regulation of cardiac rhythm, contraction and output in the face of the multiple physical and mental changes to which we are exposed throughout life.
“There is a wisdom of the head and a wisdom of the heart"
Charles Dickens (1812-1870), English writer
“Facts do not cease to exist because they are ignored”
Aldous Huxley (1894-1963), English writer and philosopher.
Sources:
1. “Decoding the molecular, cellular, and functional heterogeneity of zebrafish intracardiac nervous system”. Pedroni, A; Yilmaz, E; Del Vecchio,L; et al. Nature Communications, 2024; 15 (1) DOI: 10.1038/s41467-024-54830-w
2. Bodily changes in pain, hunger, fear, and rage; an account of recent researches into the function of emotional excitement” Cannon, W. 1915. D. Appleton and Co. USA.
3. “Mapping the little brain at the heart by an interdisciplinary systems biology team” Vadigepalli, Rajanikanth et al. iScience, Volume 24, Issue 5, 102433. https://doi.org/10.1016/j.isci.2021.102433
4. A comprehensive integrated anatomical and molecular atlas of rat intrinsic cardiac nervous system. Achanta S. et al. iScience 2020 Jun 26;23(6):101140 doi: 10.1016/j.isci.2020.101140
5. "Minimally Invasive Surgical Treatment of Atrial Fibrillation: A New Look at an Old Problem" Randall K. Wolf, Efrain A. Miranda, Operative Techniques in Thoracic and Cardiovascular Surgery, 2024, doi.org/10.1053/j.optechstcvs.2024.10.003
6 Valenza, G., Matić, Z. & Catrambone, V. The brain–heart axis: integrative cooperation of neural, mechanical and biochemical pathways. Nat Rev Cardiol 22, 537–550 (2025).
- Details
On January 23rd, 2025, I was invited to deliver a lecture on “Human Anatomical Models: History and Development of Plastination”. The lecture was delivered at the Anatomy Learning Lab which is found at the Donald C. Harrison Health Sciences Library at the University of Cincinnati.
As you may know, I am quite interested in the history of Medical Sciences and one of the topics is the history of surgical stapling. I have written extensively on this topic, including chapters in books, and the life and works of Dr. Mark M. Ravitch.
At this lecture among the attendees were several colleagues and friends and one special guest, the great granddaughter of Dr. Ravitch. Her name is Mila Colizza and she is a first year medical student here at the University of Cincinnati.
Keeping the medical tradition of the Ravitch family… Way to go Mila!!!. My best wishes in your medical career.