The persistent left superior vena cava (PLSVC) is the most common anatomical variation or anomaly in thoracic anatomy. It is present in 0 .3 to 0 .5% of the general population, but it can be present in 5% to 10% of patients who present some type of congenital cardiac malformation.
The most common presentation of this anomaly is where the PLSVC shares the venous drainage with a normal right superior vena cava. In other cases, the PLSVC is present, but there is total absence of the right superior vena cava. In these cases, the condition can be asymptomatic and can be discovered intra or preoperatively. The PLSVC is shown with a yellow arrow in the accompanying image.
In some cases, the PLSVC opens into the left atrium, causing a right to left cardiac shunt, a condition that is clearly symptomatic.
Embryologically, the development of the (right) superior vena cava begins with a similar counterpart on the left side of the embryo, the left anterior cardinal vein.
The left cardiac horn and left anterior cardinal vein eventually form the coronary sinus while its superior portion obliterates, becomes non- patent and forms the duct of Cuvier and the ligament of Marshall. A portion of the left anterior cardinal vein remains patent and forms the oblique vein of the left atrium (also known as the vein of Marshall). The vein of Marshall is found at the base of the left atrial appendage.
When present, the diameter of the PLSVC is usually quite larger than the average diameter of a normal coronary sinus, and because of the increased flow into the right atrium, the valves of Thebesius (valve at the ostium of the coronary sinus) and the valve of Vieussens (valve found at the end of the great cardiac vein and the start of the normal coronary sinus) are either absent or present with substantial reduction in size.
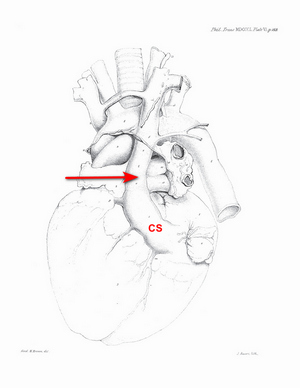
The history of the discovery and description of the PLSVC is not clear. There are many attributions, but what is undeniable is that the first complete and detailed description of this anatomical variation was done by John Marshall in 1850. The following image shows the original drawing (Plate VI) in his article “On the Development of the Great Anterior Veins Man and Mammalia; including an Account of certain remnants of Fœtal Structure found in the Adult, a Comparative View of these Great Veins the different and an Analysis of their occasional peculiarities in the Human Subject”.
While often clinically silent, PLSVC has important implications for central venous access, pacemaker lead placement, and cardiac surgery.
Personal note: My personal thanks to my good friend and contributor to "Medical Terminology Daily", Dr. Randall K. Wolf for the surgical image.
The following YouTube video by Medical Snippet with animations and drawings by Karthik Easvur provides a detailed description of the formation of the superior vena cava and the PLSVC.
Sources:
1. “Persistent left superior vena cava”. Tyrak KW, Holda J, Holda MK, Koziej M, Piatek K, Klimek-Piotrowska W. Cardiovasc J Afr. 2017 May 23;28(3):e1-e4. doi: 10.5830/CVJA-2016-084. PMID: 28759082; PMCID: PMC5558145.
2. “Persistent left superior vena cava: review of the literature, clinical implications, and relevance of alterations in thoracic central venous anatomy as pertaining to the general principles of central venous access device placement and venography in cancer patients.” Povoski SP, Khabiri H. World J Surg Oncol. 2011 Dec 28;9:173. doi: 10.1186/1477-7819-9-173. PMID: 22204758; PMCID: PMC3266648.
3. “Absent Right Superior Vena Cava and Persistent Left Superior Vena Cava: An Incidental Finding.” Joshi, Swati, and Ajmer Singh. Annals of Cardiac Anaesthesia, 2nd ed., vol. 26, no. 4, 2023, pp. 433–34, https://doi.org/10.4103/aca.aca_91_23.
4. "Absent right superior vena cava in visceroatrial situs solitus.” Bartram, U., Van Praagh, S., Levine, J. C., Hines, M., Bensky, A. S., & Van Praagh, R. 1983 Am J Card, 52(10), 1262–1268.
5. “Superior vena caval abnormalities: their occurrence rate, associated cardiac abnormalities and angiographic classification in 542 patients” Buirski, G., Jordan, S. C., Joffe, H. S., & Wilde, P. (1986). Cardiovasc Interv Rad, 9(6), 357–362.
6. "Persistent Left Superior Vena Cava with Absent Right Superior Vena Cava" Pate, Y; Gupta, R. Methodist DeBakey Cardiovasc J. 2018. 14:3. 2223-235. DOI: 10.14797/mdcj-14-3-232
7. “On the Development of the Great Anterior Veins Man and Mammalia; including an Account of certain remnants of Fœtal Structure found in the Adult, a Comparative View of these Great Veins the different and an Analysis of their occasional peculiarities in the Human Subject” 1850 Phil Trans R Soc 140:133 - 170. To download this article click here.
Video courtesy of Medical Snippet. The video, animations and drawings are the property of their owners. We encourage viewers to follow and subscribe to their respective YouTube channels.
Image of Marshall's Plate VI modified from the original. Public domain.




