Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 322 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The word [uncus] is of Latin origin and means "hook", or "curved". Its plural form is [unci]. In human anatomy we refer to hooked structures as "uncus". The the uncus of the pancreas is a hooked end segment of the head of the pancreas that curves around the superior mesenteric artery and vein. There is also the uncus of the parahippocampal gyrus, and others
The derivate root term [-unci-] gives us the adjectival form [unciform] meaning "with the shape of a hook". Applications of this root term include:
• Uncinate process of the pancreas
• Uncinate vertebral process, found in cervical vertebrae 3 to 7.
• Uncinate process of the ethmoid bone
• Uncinate gyrus, referring to the uncus of the parahippocampal gyrus
- Details
UPDATED: The term [ligament] in the abdominopelvic region has a very different meaning from the term [ligament] referring to a tendon-like structure associated with a joint. This is one of the terms that is used in different locations with different meaning.
The term [ligament] in the abdominopelvic region refers to a fold of peritoneum over an underlying structure or to a reduplication of the peritoneum. This is extremely important, as most abdominopelvic "ligaments" have a content that could be endangered through surgical manipulation.
There are many ligaments in the abdomen and pelvis. Following is a list of some of them:
- Infundibulopelvic ligament
- Ligament of Treitz
- Falciform ligament
- Round ligament of the uterus
- Median umbilical ligament
- Suspensory ligament of the sigmoid colon, etc
- Details
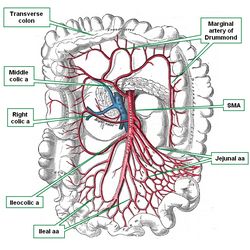
The superior mesenteric artery (SMA) is one of the anterior unpaired branches of the abdominal aorta. It is close to one centimeter in diameter at its origin and is about 15 centimeters in length. At its origin, just inferior to the celiac trunk, it is directed anteroinferiorly, hugged by the head and uncinate process of the pancreas. The SMA passes over the transverse (3rd segment) of the duodenum where it is accompanied by the inferior mesenteric vein.
The SMA provides supply to the duodenum, jejunum, ileum, the right side of the colon (cecum, vermiform appendix, and ascending colon), and the transverse colon. The jejunal and ileal arteries traverse within the layers of the mesentery.
As the SMA passes over the third portion of the duodenum, and because of the angle formed between the SMA and the abdominal aorta, it slightly compresses the duodenum. In very rare cases, this angle can be so acute as to cause duodenal obstruction requiring surgery. This rare syndrome is called “SMA compression syndrome” was first described in 1861 by Baron Carl Freiherr Von Rokitansky (1804 -1878). To see an article with a better image of the SMA-abdominal aorta angle click here.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Sir Astley Paston Cooper
Sir Astley Paston Cooper (1768 - 1841). An English anatomist and surgeon, Astley Cooper started his medical studies when he was only 16, at the St. Thomas hospital in London. He studied under Henry Cline, and later under John Hunter. Astley Cooper was a well-known anatomist, lecturer, and surgeon in his time. He is known for his many studies in abdominal hernia, otology, aneurysms, and the anatomy and diseases of the breast. In 1804 he described the abdominal transversalis fascia and the internal inguinal ring.
Born in the village of Brooke, Norfolk. At 16 years of age he was placed under the tutelage of Henry Cline (1750 - 1827), senior surgeon at the St. Thomas hospital in London for a seven-year apprenticeship. In 1789 he was appointed as an anatomy lecturer at the same hospital. In 1800 Cooper was appointed Surgeon to the Guy's Hospital in London.
He was the first to attempt the ligation of the abdominal aorta in a patient that had suffered an aortic abdominal aneurysm rupture. The patient survived for one additional day. "Astley Cooper introduced no new philosophy, policy or practice into surgery but was the perfect exponent of the scientific approach to surgery combined with skillful and successful practical ability" Brock (1969)
Cooper’s name survives in several eponymous anatomical structures and diseases he described, following are two of them:
• Cooper's ligaments of the breast: Connective tissue ligamentous strands between the pectoral fascia and the skin overlying the breast. (although it was first described by Andrea Vesalius).
• Cooper's pectineal ligament: A thickening of the periosteum on the superior aspect of the pubic bone, lateral to the pubic tubercle. This structure is a preferred site for staple positioning during a laparoscopic herniorrhaphy. When placing the staples, consideration should be placed on the potential presence of an anatomical vascular variation named the "Corona Mortis".
Although Cooper published a number of books and research papers, his seminal contribution to surgery was his two-volume "Treatise on Hernia". The first volume was published in 1795 and the second volume in 1807, with a revised second edition published in 1827.
Personal note: Although Sir Astley Cooper has been credited with the first description of the complex mammary suspensory ligaments (Cooper's ligaments), a 2016 paper by Brinkman and Hage (see Sources) contests this and gives Andreas Vesalius the honor of describing these structures nearly 300 years before Cooper! Dr. Miranda.
Sources:
1. "Sir Astley Paston Cooper." Singal, R. et al. Indian J Surg 73:1 (2011): 82-84.
2. "Sir Astley Paston Cooper, 1768-1841:the prince of surgery"Rawling, EG. Can Med Assoc J 99.5 (1968): 221.
3. "The life and work of Sir Astley Cooper" Brock, RC. Ann Royal Coll Surg England 44.1 (1969): 1-18
4. "Andreas Vesalius’ 500th Anniversary: First Description of the Mammary Suspensory Ligaments" Brinkman, RJ; Hage JJ. World J Surg (2016) 40:2144–2148
- Details
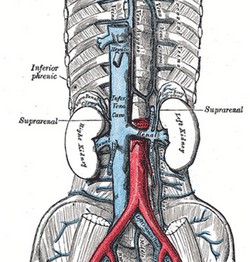
The inferior vena cava (IVC) in one of the great vessels. It brings deoxygenated blood from the lower extremities, pelvis, and areas of the abdomen to the right atrium of the heart.
As a side note, the blood returning from the digestive system does not usually enter the IVC. It has it its own venous subsystem converging into the liver by way of the portal vein.
The IVC is formed by the confluence of the right and left common iliac veins. This lower end of the inferior vena cava is found anterior to the L4-L5 intervertebral disc. The IVC covers the superior aspect of the body of L5.
The IVC ascends to the right of the abdominal aorta and anterolateral to the vertebral bodies. It receives several branches as it passes superiorly:
• Common iliac veins
• Lumbar veins
• Gonadal veins
• Renal veins
• Right suprarenal veins
• Hepatic veins
• Inferior phrenic veins
As the IVC passes posterior to the liver, it is hugged by the mass of the posterior aspect of the liver, it will receive the hepatics veins, and pass through the IVC hiatus of the respiratory diaphragm, entering immediately into the right atrium of the heart. At this point the IVC will present an incomplete venous valve known as the Eustachian valve, named after Bartolomeo Eustachius (c1500 - 1574).
Sources:
1. "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
2. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 1995
3. "Reconstructive Anatomy: A Method for the Study of Human Structure: Arnold, M WB Saunders1968
Image modified from the original by Henry VanDyke Carter, MD. Gray's Anatomy.
- Details
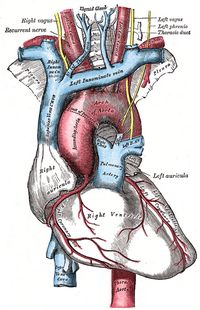
The pulmonary trunk is one of the great vessels of the heart. It is an artery that takes deoxygenated blood to the lungs as part of pulmonary circulation.
It starts proximally at the pulmonary semilunar valve. This valve is situated at superior end of the outflow tract of the right ventricle, an area called the conus arteriosus.
The pulmonary trunk has relation with the aorta on its right side, the left auricle and the left main coronary artery posteriorly. The pulmonary trunk is a short vessel, usually less than one centimeter in length. Most of the pulmonary trunk is found inside the pericardium. Almost immediately after it exits the pericardium it divides into a left and a right pulmonary artery, each one delivering deoxygenated blood to a lung.
It is a common misconception to call this vessel the "pulmonary artery". This is not correct, as the pulmonary arteries are the left and the right pulmonary arteries.
Sources:
1. "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
2. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 199
Image modified from the original by Henry VanDyke Carter, MD. Gray's Anatomy.