Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 313 guests and no members online

Jean George Bachmann
(1877 – 1959)
French physician–physiologist whose experimental work in the early twentieth century provided the first clear functional description of a preferential interatrial conduction pathway. This structure, eponymically named “Bachmann’s bundle”, plays a central role in normal atrial activation and in the pathophysiology of interatrial block and atrial arrhythmias.
As a young man, Bachmann served as a merchant sailor, crossing the Atlantic multiple times. He emigrated to the United States in 1902 and earned his medical degree at the top of his class from Jefferson Medical College in Philadelphia in 1907. He stayed at this Medical College as a demonstrator and physiologist. In 1910, he joined Emory University in Atlanta. Between 1917 -1918 he served as a medical officer in the US Army. He retired from Emory in 1947 and continued his private medical practice until his death in 1959.
On the personal side, Bachmann was a man of many talents: a polyglot, he was fluent in German, French, Spanish and English. He was a chef in his own right and occasionally worked as a chef in international hotels. In fact, he paid his tuition at Jefferson Medical College, working both as a chef and as a language tutor.
The intrinsic cardiac conduction system was a major focus of cardiovascular research in the late nineteenth and early twentieth centuries. The atrioventricular (AV) node was discovered and described by Sunao Tawara and Karl Albert Aschoff in 1906, and the sinoatrial node by Arthur Keith and Martin Flack in 1907.
While the connections that distribute the electrical impulse from the AV node to the ventricles were known through the works of Wilhelm His Jr, in 1893 and Jan Evangelista Purkinje in 1839, the mechanism by which electrical impulses spread between the atria remained uncertain.
In 1916 Bachmann published a paper titled “The Inter-Auricular Time Interval” in the American Journal of Physiology. Bachmann measured activation times between the right and left atria and demonstrated that interruption of a distinct anterior interatrial muscular band resulted in delayed left atrial activation. He concluded that this band constituted the principal route for rapid interatrial conduction.
Subsequent anatomical and electrophysiological studies confirmed the importance of the structure described by Bachmann, which came to bear his name. Bachmann’s bundle is now recognized as a key determinant of atrial activation patterns, and its dysfunction is associated with interatrial block, atrial fibrillation, and abnormal P-wave morphology. His work remains foundational in both basic cardiac anatomy and clinical electrophysiology.
Sources and references
1. Bachmann G. “The inter-auricular time interval”. Am J Physiol. 1916;41:309–320.
2. Hurst JW. “Profiles in Cardiology: Jean George Bachmann (1877–1959)”. Clin Cardiol. 1987;10:185–187.
3. Lemery R, Guiraudon G, Veinot JP. “Anatomic description of Bachmann’s bundle and its relation to the atrial septum”. Am J Cardiol. 2003;91:148–152.
4. "Remembering the canonical discoverers of the core components of the mammalian cardiac conduction system: Keith and Flack, Aschoff and Tawara, His, and Purkinje" Icilio Cavero and Henry Holzgrefe Advances in Physiology Education 2022 46:4, 549-579.
5. Knol WG, de Vos CB, Crijns HJGM, et al. “The Bachmann bundle and interatrial conduction” Heart Rhythm. 2019;16:127–133.
6. “Iatrogenic biatrial flutter. The role of the Bachmann’s bundle” Constán E.; García F., Linde, A.. Complejo Hospitalario de Jaén, Jaén. Spain
7. Keith A, Flack M. The form and nature of the muscular connections between the primary divisions of the vertebrate heart. J Anat Physiol 41: 172–189, 1907.
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
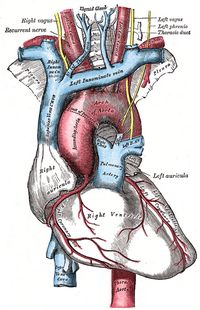
The superior vena cava (SVC) is one of the great vessels, a large vein that receives the venous return from the upper portion of the body, including the head and neck, upper extremities, and chest, with some venous return from the posterior aspect of the abdomen. The exception is the venous return of the heart which comes back by way of the coronary veins and coronary sinus.
The SVC originates at the junction of the left brachiocephalic vein with the right brachiocephalic vein. Its origin is described at the lower border of the first rib. The SVC ends at the cavoatrial junction, where it empties into the right atrium of the heart. It is here at the cavoatrial junction that anatomists describe a small horseshoe-shaped structure, the sinoatrial node or SA node, part of the conduction system of the heart.
The length of the SVC is between 6 to 8 cm. There are many anatomical variations of the superior vena cava, as described here.
The arch of the azygos vein empties into the posterior aspect of the SVC. The arch of the azygos vein receives the venous return of the azygos and hemiazygos venous systems, including the venous return of the posterior intercostal veins, and the ascending lumbar veins.
Sources:
1. "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
2. "Gray's Anatomy" 38th British Ed. Churchill Livingstone 1995
Image modified from the original by Henry VanDyke Carter, MD. Gray's Anatomy.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Juan Vucetich (1858–1925)
Personal note: When working on the root term [-dactyl-] I came upon the biography of Juan Vucetich, the individual who created the modern method of dactyloscopy. Even though not a physician or anatomist, his life and accomplishments deserve to be presented here. Dr. Miranda.
Juan Vucetich (1858–1925) Juan Vucetich was born Ivan Vučetić in Croatia. In 1882, at 24 years of age he immigrated to Argentina, where he adopted the Spanish translation of his Croatian name. Because of his literacy (I have found no information on his actual studies), he started to work at the Argentinian Sanitary Works until he transferred to the Police Department Office of Identification and Statistics.
Vucetich was placed in charge of the anthropometric method used at the time to identify criminals based on bodily measurements. After reading an article in a French journal on Francis Galton's experiments with fingerprints as a means of identification, Vucetich began collecting fingerprints, taken from arrested men, while also making Bertillon-style anthropometric measurements. Galton's initial study proposed 40 parameters to classify fingerprints, but no system to collect or identify and individual using only this method.
He soon devised a useable system to group and classify fingerprints, which he called "Ichnophalangometrics" (description of phalangeal measurements). Thankfully, that name was later changed to dactyloscopy
Vucetich demonstrated the utility of fingerprint evidence in an 1892 case, which resulted in the identification and conviction of a suspect for first-degree murder. Shortly after that, he dismissed entirely the Bertillon anthropometric system, arguing that a full ten-finger set of fingerprints was sufficient for identification, and that complicated anthropometric measurements were unnecessary.
In 1900, the Argentine Republic began issuing a kind of internal passport which included fingerprints—a practice that was eventually adopted by many other countries. The 1904 publication of "Dactiloscopía Comparada", Vucetich's definitive work on fingerprint identification, and his travels to other countries, helped to spread his system throughout the world. Today, the Argentinian Police Academy is named after Juan Vucetich
Sources:
1. "Juan Vucetich and the origins of forensic fingerprinting". Visible Proofs. National Library of Medicine
2. Vucetich, Juan. Dactiloscopia comparada: El nuevo sistema argentino. Tip. Jacobo Peuser, 1904
- Details
The prefix [semi-] originates from the Latin [semis] meaning "half". Applications of this prefix include:
- Semicomatose: Not completely in a coma, half in, half out
- Semimembranous: The name of a muscle that is half membranous (tendinous), half muscle
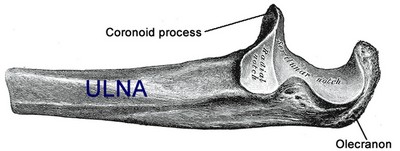
- Semilunar: With the shape of a half-moon, as the semilunar area of the olecranon
- Semicartilaginous: Half formed by cartilage
- Details
The [olecranon] is the bony prominence of the elbow, that what some call "the funny bone". It is hook-shaped and has a semilunar (half-moon shaped) area which forms part of the elbow joint, articulating with the trochlea of the humerus.
Covered by a bursa, the olecranon receives the distal attachments of the triceps brachii muscle and the anconeous muscle.
Click for a larger image
The word [olecranon] originates from the mixing of two Greek words [ωλένη] (oleni) meaning "ulna" and the word [κρανίοmeaning "head", or "cranium". Literally, "the head of the ulna"
Note: The links to Google Translate in these articles include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
- Details
The root term [-galact-] originates from the Greek [γάλα] (gala) meaning "milk". The use of this Greek word can be seen in the word [galaxy] initially used to refer to the Milky Way, our own galaxy. Applications of this include:
- Galactorrhea: The suffix [-(o)rrhea] means "flow" or "discharge". A discharge of milk
- Galactocyte: The suffix [-(o)cyte] means "cell". A milk-producing cell
- Galactophorous: A conduit or tube that carries milk
- Galactophoritis: An inflammation or infection of a conduit or tube that carries milk
- Galactopoiesis: The suffix [-(o)poieisis] means "to make", "action", "process". or "performance.. Refers to the process that creates milk
Note: The links to Google Translate include an icon that will allow you to hear the Greek or Latin pronunciation of the word.
- Details
The medical suffix [-(o)rrhea] has a Greek origin and means "flow" or "discharge". The term is used in many medical words. Applications of this root term include:
- Galactorrhea: The root term [-galact-] means "milk". Milk discharge
- Agalactorrhea: The suffix [a-] means "without" or "absence". Absence of milk discharge
- Diarrhea: The root term [-dia] means "complete" or "trough". The word needs no explanation
- Amenorrhea: The root term [-men-)] means "menses". Absence of menstrual flow
- Dacryohemorrhea: A bloody flow of tears