Medical Terminology Daily (MTD) is a blog sponsored by Clinical Anatomy Associates, Inc. as a service to the medical community. We post anatomical, medical or surgical terms, their meaning and usage, as well as biographical notes on anatomists, surgeons, and researchers through the ages. Be warned that some of the images used depict human anatomical specimens.
You are welcome to submit questions and suggestions using our "Contact Us" form. The information on this blog follows the terms on our "Privacy and Security Statement" and cannot be construed as medical guidance or instructions for treatment.
We have 416 guests online

Georg Eduard Von Rindfleisch
(1836 – 1908)
German pathologist and histologist of Bavarian nobility ancestry. Rindfleisch studied medicine in Würzburg, Berlin, and Heidelberg, earning his MD in 1859 with the thesis “De Vasorum Genesi” (on the generation of vessels) under the tutelage of Rudolf Virchow (1821 - 1902). He then continued as a assistant to Virchow in a newly founded institute in Berlin. He then moved to Breslau in 1861 as an assistant to Rudolf Heidenhain (1834–1897), becoming a professor of pathological anatomy. In 1865 he became full professor in Bonn and in 1874 in Würzburg, where a new pathological institute was built according to his design (completed in 1878), where he worked until his retirement in 1906.
He was the first to describe the inflammatory background of multiple sclerosis in 1863, when he noted that demyelinated lesions have in their center small vessels that are surrounded by a leukocyte inflammatory infiltrate.
After extensive investigations, he suspected an infectious origin of tuberculosis - even before Robert Koch's detection of the tuberculosis bacillus in 1892. Rindfleisch 's special achievement is the description of the morphologically conspicuous macrophages in typhoid inflammation. His distinction between myocardial infarction and myocarditis in 1890 is also of lasting importance.
Associated eponyms
"Rindfleisch's folds": Usually a single semilunar fold of the serous surface of the pericardium around the origin of the aorta. Also known as the plica semilunaris aortæ.
"Rindfleisch's cells": Historical (and obsolete) name for eosinophilic leukocytes.
Personal note: G. Rindfleisch’s book “Traité D' Histologie Pathologique” 2nd edition (1873) is now part of my library. This book was translated from German to French by Dr. Frédéric Gross (1844-1927) , Associate Professor of the Medicine Faculty in Nancy, France. The book is dedicated to Dr. Theodore Billroth (1829-1894), an important surgeon whose pioneering work on subtotal gastrectomies paved the way for today’s robotic bariatric surgery. Dr. Miranda.
Sources:
1. "Stedmans Medical Eponyms" Forbis, P.; Bartolucci, SL; 1998 Williams and Wilkins
2. "Rindfleisch, Georg Eduard von (bayerischer Adel?)" Deutsche Biographie
3. "The pathology of multiple sclerosis and its evolution" Lassmann H. (1999) Philos Trans R Soc Lond B Biol Sci. 354 (1390): 1635–40.
4. “Traité D' Histologie Pathologique” G.E.
Rindfleisch 2nd Ed (1873) Ballieres et Fils. Paris, Translated by F Gross
"Clinical Anatomy Associates, Inc., and the contributors of "Medical Terminology Daily" wish to thank all individuals who donate their bodies and tissues for the advancement of education and research”.
Click here for more information
- Details
The medical term [epistaxis] refers to a “nose bleed”.
It is considered to be a Modern Latin term that originates from the Greek word [επίσταξη] (epístaxí). The word is composed of [επί] [epi-] meaning "on", "upon", or "above", and [στάζει] (stázei), meaning "in drops", "dripping".
The term was first used by Hippocrates, but only as [στάζει] , to denote dripping of the nose, and was later changed to [επίσταξη] to denote “dripping upon”. The term itself does not include or denote that the blood loss is from the nose, but its meaning has been implied and accepted for centuries. The plural form for epistaxis is epistaxes.
Skinner (1970) says that the term was first used in English in a letter by Thomas Beddoes (1760-1808) in a letter to Robert W. Darwin (1766-1848) in 1793. Robert Darwin was an English physician, father or Charles Darwin (1809-1882) author of “The Origin of the Species”.
Sources:
1. "The Origin of Medical Terms" Skinner, HA 1970 Hafner Publishing Co.
2. "Medical Meanings - A Glossary of Word Origins" Haubrich, WD. ACP Philadelphia
Note: The links to Google Translate include an icon that will allow you to hear the pronunciation of the word.
- Details
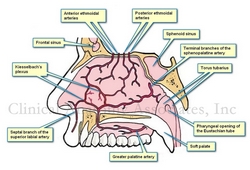
Kiesselbach's plexus is named after Dr. Wilhelm Kiesselbach (1839 – 1902), a German otolaryngologist. It is an area in the anteroinferior aspect of the nasal septum where several arteries from different origins meet and anastomose.
This arterial plexus is also known as the "locus Kiesselbachii, Kiesselbach's triangle, or Little's plexus, or Little's area. This area of the anteroinferior nasal septum has a propensity for epistaxis or nasal bleeding. In fact, close to 90% of nose bleeds (epistaxes) happen in this area.
There is a secondary area where epistaxis may happen, but this is a venous nose bleed. This is Woodruff's plexus, a venous plexus found in the posterior aspect of inferior turbinate on the lateral wall of the nose.
Thanks to Jackie Miranda-Klein for suggesting this post.
- Details
- Written by: Efrain A. Miranda, Ph.D.
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Letter from Ephraim McDowell
to Robert Thompson
As some of you may know by now, I am a collector of antique medical books and books that relate to the history of anatomy and medicine.
As important as the books themselves are, there are details beyond the book itself that can take hours of my time doing research. The first one is the bookplates (also known as Ex-Libris). The have been used for centuries by book owners and collectors to identify the books in their collections, a tradition that seems to be falling in disuse. Not me, I have one that you can see here. Some of these can lead to places that you cannot imagine initially. One of these bookplates took me to research a potential resident ghost in a library!
Provenance is also important. Where was it printed? Who owned it? Who was the illustrator? etc. I recently acquired a second copy of the book “EPHRAIM MCDOWELL, FATHER OF OVARIOTOMY AND FOUNDER OF ABDOMINAL SURGERY. With an Appendix on JANE TODD CRAWFORD”. By AUGUST SCHACHNER, M.D. Cloth, 8vo.A p. 33I. Philadelphia, J. B. Lippincott CO., I921. Dr. McDowell has also been featured in this blog in the series "A Moment in History".
This second copy is most valuable because of the papers found within the book. There is a series of notes, newspaper clippings, and copies of letters! Here is a detail of what I have found:
The book seems to have belonged to Cecil Stryker, MD.,a physician in Cincinnati, and one of the founders of the American Diabetes Association (ADA). There is a copy of a letter by Dr. Ephraim McDowell to Dr. Robert Thompson (Sr.) dated January 2nd, 1829, a year before Dr. McDowell's death. The letter is shown in the image attached. In this letter Dr. McDowell describes in his own words the ovariotomy he performed on Jane Todd. He also describes other ovariotomies he performed and his opinion on "peritoneal inflammation".
There is a note from Dr. Cecil Striker to "Bob" dated 6/3/73 when he gifted a copy of this book. In the note Dr. Striker explains that he bought several copies of the book and he is sending this copy to him. There is also a copy of Dr. McDowell's prayer (costs 25 cents), and a page of the Kentucky Advocate newspaper published in Danville, KY and dated Sunday April 15, 1973 on the restoration of Dr. Alban Goldsmith home, a surgeon who assisted Dr. McDowell in his first ovariotomy (first in the world, that is).
Last, there is a note dated September 16, 1974 from the wife of Dr. West T. Hill, Chairman of the Dramatic Arts Department at Centre College in Danville, Kentucky. In this handwritten note she mentions the McDowell family reunion that took place on June 15 and 16, 1974 in Danville. With the note comes the program and registration form for the festivities! Dr. West T. Hill was one of the many responsible for the restoration of the MacDowell Home and Museum. Today Danville has the West T. Hill community theatre that honors his name.
All of this in one book, as I always say "You know where you are going to start reading it, but you never know where are you going to end in researching it". This book will be a great addition to my library catalog. Dr. Miranda.
- Details
Rudi Coninx, MD is a physician and Chief a.i. Humanitarian policy and Guidance at the World Health Organization (WHO), based in Geneva. He obtained his MD from the University of KU Leuven Belgium, a Doctorate in Tropical Medicine from the Prins Leopold Instituut voor Tropische Geneeskunde, and an MPH from the John Hopkins University School of Medicine.
His CV shows more than twenty five years of national and international experience in policy and strategy development and analysis, policy dialogue, technical advice and program management support to countries and WHO country offices. Considerable experience in strengthening WHO country offices and in working with partners and networks at the global as well as filed level. Coordinated the WHO Country Focus Policy for more than five years and worked as a member in various strategic planning, decentralization, and global and regional partnership groups, including national and international committees, taskforces. Published several articles on policy analysis, management and health and development in regional and international journals.
He is also an Associate Faculty, Bloomberg School of Public Health, Johns Hopkins University, USA.
He has held a series of positions with the International Committee of the Red Cross, and also within the World Health Organization. His LinkedIn profile can be found here.
Thanks to Dr. Coninx for taking time of his busy schedule and collaborating with "Medical Terminology Daily" with the article "Did Andreas Vesalius really die from scurvy?" which he co-authored with Theo Dirix. We look forward to his future writings in this blog.
- Details
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Wilhelm Kiesselbach
Wilhelm Kiesselbach (1839 – 1902) German otolaryngologist born in the city of Hanau. Started his medical studies in 1859 in Göttingen. Marburg, and Tübingen. Because of an accident that affected one of his hands and legs, his doctorate was delayed until 1875.
He specialized in otolaryngology in Vienna, although he also studied and specialized in ophthalmology. He had a number of positions such as assistant professor at the Medical Polyclinic in Erlangen, assistant professor for ophthalmological examinations at the Surgical Clinic in Erlangen, and senior physician for ophthalmology.
He died of an infection he contracted while working with patients at the clinic.
His name is eponymically tied to the locus Kiesselbachii, also known as Kiesselbach’s plexus, an area of the anteroinferior nasal septum known for propensity for epistaxis or nasal bleeding. In fact, close to 90% of nose bleeds happen in this area. in this region, terminal branches of the anterior ethmoid artery, greater palatine artery, sphenopalatine artery and superior labial artery anastomose forming a plexus.
- Details
- Written by: Pavlos Plessas
NOTE: In 2014 Pavlos Plessas presented the compelling theory that Andreas Vesalius died in 1564 from scurvy on the island of Zakynthos. With his permission his original article entitled "Powerful indications that Vesalius died from scurvy" was published in this blog in 2016.
His theory was later challenged by Theo Dirix and Dr. Rudi Coninx in this same blog with the article "Did Andreas Vesalius really died from scurvy?". Pavlos Plessas' rebuttal to the latter article is published here from a letter to Theo Dirix.
...continued from: An answer regarding the death of Andreas Vesalius (2). For the initial article, click here.

Pavlos Plessas
Click on the image for author information
16. The study’s sample is small, not representative of a general population, based on answering a questionnaire and not observation
Clinical studies of this nature face obvious limitations. If the authors are prepared to disbelieve the testimony of people who lived in a confined space with many victims of scurvy until the final fatal outcome, it is no wonder they complain about the study. Doubting is their prerogative, however, the way to discredit the study is to either find an error in the data or its interpretation, or conduct their own study and come up with different results.
17. The quoted personality changes peak on day 107. Certainly not an early symptom
Do the authors consider a symptom only when it peaks? Is pain not pain until it becomes unbearable?
18. Elevation of this triad is also found in prolonged semi starvation, and deficiencies of B-complex vitamins
The study at this point refers to Brozek and indirectly to the Minnesota Starvation Experiment of 1944-45, meaning semi-starvation over many months. It is clearly not relevant here as Vesalius did not face food shortages for more than a few weeks. As for vitamins of the B complex if the authors are ready to suggest that Vesalius may have died from beriberi or pellagra I am ready and happy to argue.
19. These changes are characteristic of individuals who are physically ill, as the subjects were
Yes, but in the beginning they did not know that they were ill (no clinical signs). Besides, there is another study which indicates that “behavioural change in human scurvy patients has a physiological rather than a solely psychological basis” (6). And there is a suggested biological explanation. “Vitamin C is a cofactor in the biosynthesis of catecholamines, most notably in the conversion of dopamine to norepinephrine, which may explain the behavior and mood disorders associated with vitamin C deficiency” (7). “Acutely hospitalized patients experience emotional distress for many reasons; therefore, it may seem unexpected that simple correction of their vitamin C deficiency could account for such rapid and dramatic improvements in psychological well-being. There are several reasons why this possibility merits serious consideration. First, the result is biologically plausible. Psychological dysfunction is known to occur in vitamin C deficiency, presumably because of the involvement of ascorbate in neuronal transmission and in brain neurotransmitter and fuel metabolism.” (8)
20. Vesalius’ reaction was normal in the view of many passengers getting sick, dying and being thrown overboard
Did all the passengers start begging the crew not to throw their dead bodies overboard? Did Boucherus do it? Why did he then only report Vesalius doing it? Was it normal behaviour for a distressed 16th century aristocrat to beg lowly-born sailors?
21. The only known symptoms of Vesalius are consistent with many other diseases
I think the best way for someone to debunk the scurvy theory is to make a list of diseases that could have killed Vesalius. It appears that the authors do not consider it too great a challenge. But these diseases have to be compatible with the circumstances and the authors will have to do considerably better than the suggestion of food poisoning.
22. Vesalius died from exhaustion combined by illness
All sources agree that Vesalius died from an illness. He had gone through an ordeal, he was probably malnourished and dehydrated to some extent but there is no evidence of exhaustion. He was sick, not tired. He was a passenger on a ship, not a galley slave. The crew, who worked around the clock, were fine. The only exhaustion was that of his reserves of Vitamin C.
23. In order to have a definite diagnosis, it will be important to locate the grave of Andreas Vesalius
Amen. I have one more reason to wish it than most of the many people who wish Theo and Pascale good luck in the search for the grave. I expect to be vindicated. And I hope that maybe my work will contribute in the beyond doubt identification of Vesalius’ remains..
Sources:
1. "Voyages and Travels in the Levant in the Years 1749, 50, 51, 52" London 1766, p. 147
2. "Medicina Nautica: an Essay on the Diseases of Seamen" Volume III, London 1803, p. 387
3. "De magnis Hippocratis" Lienibus Libellus, Antwerp 1564, pp. 26a – 31b
4. A voyage round the world in the years MDCCXL, I, II, III, IV, 5th edition, London 1749, p. 101.
5. Robert A. Kinsman and James Hood, Some behavioral effects of ascorbic acid deficiency, The American Journal of Clinical Nutrition, April 1971.
6. Fiona E. Harrison, Behavioural and neurochemical effects of scurvy in gulo knockout mice, Journal for Maritime Research, Volume 15, Issue 1, 2013.
7. Olivier Fain, Musculoskeletal manifestations of scurvy, Joint Bone Spine 72, 2005.
8. Wang et al, Effects of vitamin C and vitamin D administration on mood and distress in acutely hospitalized patients, the American Journal of Clinical Nutrition, 2013.
PERSONAL NOTE: My thanks to all the authors who are part of this ongoing discussion and who are also friends and contributors to this blog. Everybody is correct in the fact that the only way to find the truth of the cause of death of Andreas Vesalius is to find his grave. The quest is ongoing and hopefully we are closer every day to this objective. Dr. Miranda