The [internal thoracic artery] is a bilateral artery of the thorax and is known to many as the [internal mammary artery], although this is not its proper anatomical name.
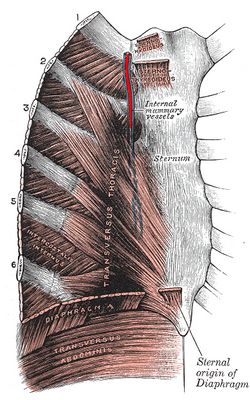
The internal thoracic artery is the first branch to arise off the subclavian artery. It descends inferiorly in a parasternal position, on the posterior aspect of the anterior thoracic cage. It is in contact with the ribs and as it descends it is covered posteriorly by the transversus thoracis muscle.
At the level of the sixth costal cartilage the internal thoracic artery gives off the musculophrenic artery and changes its name, continuing inferiorly as the superior epigastric artery. This artery will pass through one of the hiatuses of the respiratory diaphragm and in turn will become the inferior or deep epigastric artery at the level of the umbilicus. The deep epigastric artery (one of the boundaries of Hesselbach's triangle) will in turn open into the external iliac artery. The internal thoracic artery is part of a longitudinal collateral circulation arterial channel that parallels the aorta.
The internal thoracic artery will give off several branches. The first one is usually the pericardiacophrenic artery, a long artery that descends with the phrenic nerve alongside the parietal pericardium providing blood supply, as its name implies, to the pericardium and the phrenic nerve. Other branches are the anterior intercostal arteries, which communicate with the posterior intercostal arteries and the aorta.
The internal thoracic artery also gives arterial branches to the sternum and provides superficial, perforating branches to the medial side of the breast, hence its clinical name, the internal mammary artery.
The internal thoracic artery can be used to create a cardiac graft when performing a Coronary Artery Bypass Graft (CABG). Because of the two names used to denote this artery, surgeons will refer to the procedure either as a ITA (internal thoracic artery) or an IMA (internal mammary artery) CABG.